Abstract
Background: Morphologic complete remission (CR) is the gold standard for assessing response in acute leukemia. Patients who achieve CR with incomplete count recovery (CRi) in acute myeloid leukemia typically have inferior overall survival and lower event free survival (Walter et al, JCO 2010 and Chen et al, JCO 2015). Incomplete hematologic recovery is likely not an independent risk factor for inferior outcome but possibly correlates with adverse disease characteristics such as high risk cytogenetics or minimal residual disease post therapy. Furthermore, remission status prior to allogeneic stem cell transplantation (SCT) is an important predictor of post-transplant outcome. However, the prognostic role hematologic recovery carries prior to allogeneic transplantation for acute leukemia is not known.
Aim: To study the impact of CRi with corresponding impact on relapse incidence (RI), non-relapse mortality (NRM) and overall survival (OS) in allogeneic SCT for acute leukemia.
Methods: Patients with acute myeloid or lymphoid leukemia who received allogeneic SCT at our institution between 2010-2015 were identified. All clinical and pathologic data were retrospectively extracted. All patients were deemed in morphologic remission at the time of transplant without evidence of active disease. CR and CRi were defined in accordance to previous international working group definitions. Categorical and continuous variables were analyzed using Pearson's chi-squared and Wilcoxon / Kruskal-Wallis, respectively. Survival estimates were calculated using the Kaplan-Meier and log-rank test. RI was estimated accounting NRM on a competing event analysis using Grey's model.
Methods: Patients with acute myeloid or lymphoid leukemia who received allogeneic SCT at our institution between 2010-2015 were identified. All clinical and pathologic data were retrospectively extracted. All patients were deemed in morphologic remission at the time of transplant without evidence of active disease. CR and CRi were defined in accordance to previous international working group definitions. Categorical and continuous variables were analyzed using Pearson's chi-squared and Wilcoxon / Kruskal-Wallis, respectively. Survival estimates were calculated using the Kaplan-Meier and log-rank test. RI was estimated accounting NRM on a competing event analysis using Grey's model.
Results:
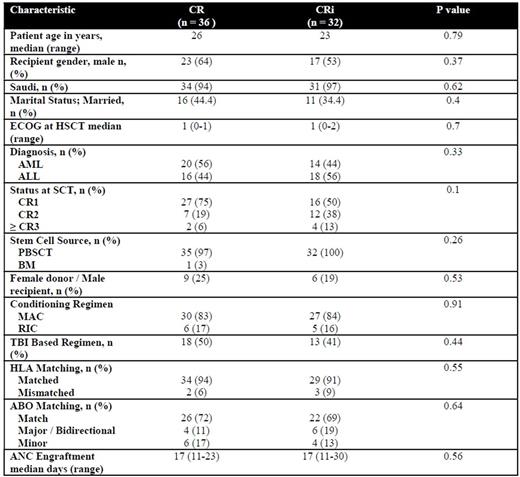
A. Baseline characteristics: A total of 68 patients were identified. A total of 36 were in CR while 32 were in CRi. Baseline patient, disease and transplant characteristics stratified by group are shown (Table 1). Importantly, there were no significant differences between the cohorts with regards to gender, disease status at SCT, intensity of conditioning regimen, use of total body irradiation (TBI), HLA and ABO matching.
B. Transplant outcomes: Median follow up of the entire cohort was 13.6 (2-64.9) months. During which 2-year rates of RI, NRM and OS were 42.4, 12.8% and 63.9%, respectively. Stratified by count recovery, the 2-year rates of RI for CR and CRi were 36.2 vs. 43.1, respectively (p = 0.39). 2-year NRM for CR and CRi were 21.7% vs. 11%, respectively (p = 0.1). 2-year OS for CR and CRi were 59% vs. 61.8%, respectively (p = 0.58).
Conclusion: We observed comparable post-transplant outcomes between CR and CRi. This suggests that in contrast to acute myeloid leukemia, SCT had a role in mitigating the negative prognostic implication of CRi. These results could have implications as physicians may not need to postpone SCT to await hematologic recovery. This important question should be further validated in a larger cohort of patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal