Abstract
Introduction:Acute Graft-versus-Host Disease (aGVHD) is a frequent complication of Allogeneic Hematopoietic cell transplants (allo-HCT); aGVHD, especially Grade III-IV, can be lethal with increased morbidity and mortality and can occur in upto 40-50% of allo-HCT. GVHD prophylaxis has been used for control of GVHD, with use of calcineurin inhibitors, anti-metabolites and anti T cell antibodies. Use of Post-transplant Cyclophosphamide (PTCy) has recently been used extensively in haplo-identical transplant setting with promising results. However, PtCy has mainly been used in patients with BM as the stem cell source. In those patients with PBSC as the stem cell source, alone PTCy has been associated with clinically significant acute and chronic GVHD. As most of our patients use PBSC as the graft source, we hypothesized to combine both ATG and PTCy to reduce incidence of both acute and chronic GVHD in our patient cohort. Here we present a small cohort data using a combination of all these agents to effectively reduce aGVHD in hematological malignancies..
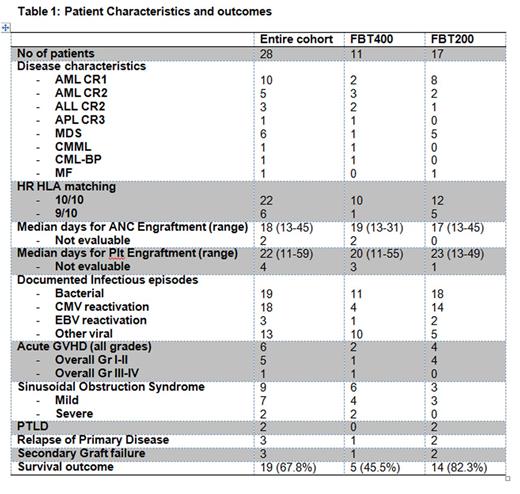
Methods:A total of 28 patients with hematological malignancies, who had an unrelated donor underwent allo-HCT at our center from 1 Oct 2015 to 31 Mar 2016. The characteristics of the patients are summarized in Table 1. The conditioning regimen was either myeloablative (MAC, namely FBT400) or Reduced Intensity (RIC, namely FBT200) in patients with age ≤ 60 and >60 years, respectively. After interim analysis when increased non-hematological toxicity was observed in the MAC arm, all patients subsequently received FBT 200 conditioning. Peripheral blood was used as the stem cell source in all patients. Filgrastim was used from day +7 onwards for 13 patients. Special emphasis was given to incidence of acute GVHD, infections, regimen related toxicities and engraftment.
Results:Out of total of 28 patients, aGVHD was seen in only 6 (21.4%) patients, five of which had skin involvement (Grade I-II) and one suspected liver involvement (Grade III), all of which responded rapidly to steroids. However, we did observe increased toxicities such as sinusoidal obstruction syndrome (32%), bacterial infections (68%) and viral infections (46%; CMV reactivations in 64%). Primary disease relapse, secondary graft failure and EBV reactivations were seen in 10% of cases, with documented Post Transplant Lymphoproliferative Disorder (PTLD) in only 2 patients. The overall survival of the entire cohort was 67.8% with a median duration of 6 months (range; 3-8 months). In comparison to MAC, RIC regimen was found to be superior with no Gr III-IV aGVHD, less toxicity and improved survival (RIC-82% vs MAC-45%).
Conclusions: Combination of ATG-PTCy-CsA is an effective strategy to reduce aGVHD in unrelated donor transplants, albeit with moderate increase in toxicities. RIC with this combination was associated with less organ damage and superior survival. However, a long term follow up is needed to assess relapse and cGVHD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal