Abstract
Background
In younger and fit multiple myeloma (MM) patients (pt), autologous stem cell transplantation (ASCT) remains the gold standard treatment.
Mobilization chemotherapy is usually administered in an inpatient regimen and Cyclophosphamide (CY) at different doses is the most used chemoterapy for collecting peripheral blood stem cells (PBSC) in MM. Clinical trials have demonstrated that intermediate dose CY (3 and 4 g/m2, ID-CY) combined with G-CSF, is an efficient mobilizing regimen with less toxicity compared with high dose CY (7 g/m2, HD-CY) in term of neutrophil recovery, thrombocytopenia, need of transfusions and IV antibiotics. (Fitoussi et al, BMT 2001; Goldschmidt et al, BMT 1996).
Objective
To evaluate the safety of mobilization therapy administered in an outpatient regimen, with the prospect to lower costs and minimize patient inconvenience, maintaining an optimal yield.
Methods
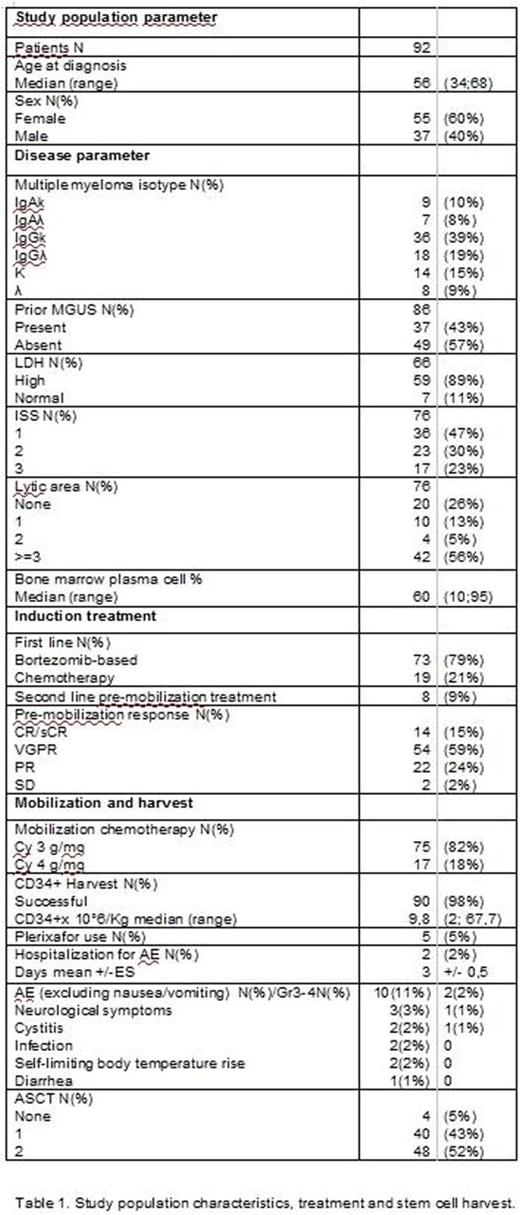
92 pt with newly diagnosed MM underwent outpatient stem cell mobilization between 2002 and 2016 with CY 3 g/m2 (82%) or 4 g/m2 (18%) + G-CSF after induction therapy with bortezomib-based (79%) or VAD-like (21%) regimens. No antibiotics prophylaxis was routinely used. Day 0 was defined as the CY infusion day. CY was administered in 2-4 consecutive 1h infusions (depending on total dose). Hyper-hydration (3.5/4 l), antiemetics and the uroprotectant Uromitexan were began IV 1 hour before CY infusion. Subsequently, Uromitexan was continued at home orally in the next 12h. Furthermore, the patient was advised to drink 2.5/3 l of water in the next 24h. G-CSF 10 mcg/Kg was started by day +5 and continued until completion of apheresis. Blood count was monitored at day + 4 and daily from day +7. CD34+ cells were counted on peripheral blood by day 7; apheresis was started at leukocyte rise and with a value of at least 20 CD34+/μl. Number of apheresis depended on the number of CD34+ cells collected to obtain al least 4x106 CD34+/Kg.
Results
Median age at diagnosis of was 56y (range 34-68). MM isotype was IgA, IgG and micromolecular respectively in 18%, 58% and 24%. Prior MGUS was present in 37 cases (43%). LDH was elevated in 7 pt (11%), whereas ISS was 1/2/3 in 47%/30%/23%. Bone disease was detectable in 74% of pt, with 56% having 3 or more osteolysis. Median bone marrow plasma cell at diagnosis was 60% (range 10-95%).
Pt received induction with bortezomib-based regimens (79%) or chemoterapy, mostly VAD (21%). 8 pt (9%) required second line therapy before mobilization. Response prior of mobilization was CR/sCR in 15%, VGPR in 59%, PR in 24%, and SD in 2%.
Stem cell collection was successful in 98% of pt, with a median CD34+ harvest of 9.8x106/Kg.
Chemotherapy was very well tolerated. Most frequently observed adverse events (AEs) were nausea and vomiting of grade 1-2. 2 pt experienced cystitis (one grade 1, one grade 2), 2 pt infections, 2 pt hyperthermia regressed rapidly without therapy, 1 patient diarrhea. 3 pt had neurological symptoms: in 2 cases they were aspecific (headache, instability); the other case presented a sudden appearance of 7th cranial nerve deficit at the end of mobilization chemotherapy infusion with negative imaging and successively regressed in few hours, interpreted as transient ischemic attack not correlated with Cy. Only 2 patient required hospitalization for AEs: 1 patient for fever grade 3 without microbiological findings, rapidly regressed with IV antibiotics; the second one for 7th cranial nerve deficit. These were the only grade 3 AEs, no grade 4 AEs verified. There were no other significant AEs related to chemotherapy.
All pt except 2 proceeded to stem cell harvest and reached CD34+ target, but 5 pt required administration of Plerixafor on demand. The 2 pt not reaching CD34+ target successfully mobilized afterwards, 1 with different chemoterapy and the other with G-CSF and Plerixafor. After mobilization, 88 pt proceeded to single (45%) or double (55%) ASCT.
Conclusion
In conclusion, outpatient mobilization with ID-CY appears to be an efficient and safe procedure, with minimal and manageable side effects and low rate of hospitalization. Outpatient mobilization could ameliorate the quality of life of pt and reduce costs, avoiding or minimizing the hospitalization rate, without compromising the safety profile and the success of PBSC collect.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal