Abstract
Background: Glucocorticoids has been a backbone of various treatment regimens for multiple myeloma (MM). The repeated and chronic use of high doses of glucocorticoids is associated with development of secondary adrenal insufficiency (AI), and AI could be a major problem in critically-ill patients. However, there has been no specialized data about incidence and clinical significance of secondary AI in hospitalized patients with MM.
Purpose: The objective of this retrospective study is to evaluate incidence, predictive factors, and clinical significance of secondary AI in hospitalized patients with MM.
Methods: We retrospectively evaluated medical records of MM patients who were hospitalized in Chonnam National University Hwasun Hospital, South Korea from December 2014 to December 2015. The definite AI was diagnosed when the peak cortisol concentration was less than < 500 nmol/L (18 mcg/dL) after ACTH administration.
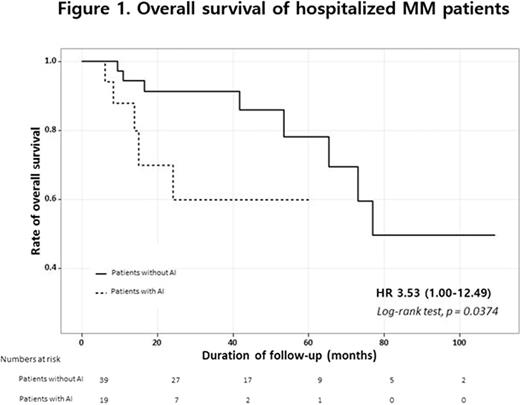
Results: Between December 2014 and December 2015, 77 patients were hospitalized, and 58 underwent rapid ACTH stimulation test. The most frequent cause of hospitalization was infection (70.7%), followed by weakness (24.1%), and the others (5.3%). The definite AI was confirmed in 19 patients (32.7%). To evaluate the predictive factors of AI, all variables including clinical characteristics, laboratory results, cumulative steroid dose, and treatment duration at hospitalization were analyzed, but there were no significant predictors for AI. In addition, the patients with AI had a significantly poor survival outcomes compared to those without AI (the median overall survival of 42.3 months vs. 82.7 months; P = 0.037) (Figure 1).
Conclusions: This study showed that the secondary AI is not a rare condition among hospitalized patients with MM, and there was no specific predictable symptoms or signs. In addition, development of AI in the treatment period is associated with a poor prognosis. This study suggests that evaluation of AI is routinely needed in hospitalized patients with MM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal