Abstract

Background: Cytogenetic evaluation using fluorescence in situ hybridization (FISH) at the time of diagnosis is essential for initial risk stratification in multiple myeloma. The presence of specific cytogenetic abnormalities is known to confer a poor prognosis, less is known about the cumulative effect of multiple cytogenetic high-risk abnormalities. We aimed to evaluate the prognostic implications of the presence of multiple cytogenetic high-risk abnormalities at the time of diagnosis.
Methods: We studied 226 patients who were diagnosed with multiple myeloma between July 2004 and July 2014 at Mayo Clinic Rochester, underwent FISH evaluation within six months of diagnosis, and presented with cytogenetic high-risk abnormalities. High-risk cytogenetics were defined as t(4;14), t(14;16), t(14;20), del(17p), or gain(1q). Bone marrow aspirates were evaluated for deletions, monosomies, trisomies, and tetrasomies using chromosome- or centromere-specific FISH probes. IGH rearrangements were evaluated using an IGH break-apart probe and evaluating up to five potential partners (FGFR3, CCND1, CCND3, MAF, and MAFB). Kaplan-Meier overall survival estimates were calculated and the log-rank test was used to compare overall survival in patients with single and multiple cytogenetic high-risk abnormalities. A multivariable-adjusted Cox regression model was used to assess the effect of multiple cytogenetic high-risk abnormalities on overall survival adjusting for age, sex, and Revised International Staging System (R-ISS) stage. P-values below 0.05 were considered statistically significant.
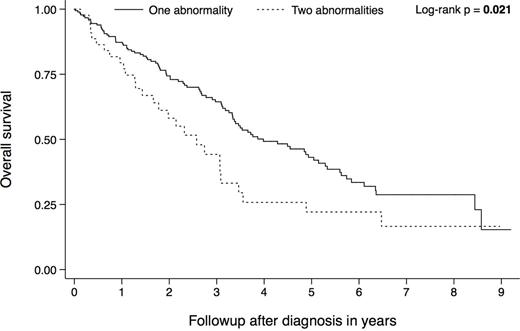
Results: The median age at diagnosis was 65 years (32 - 90), 129 (57%) of the patients were male. The median overall survival was 3.5 years (3.1 - 4.9) for the entire cohort (n = 226), 4.0 years (3.3 - 5.1) for those with one cytogenetic high-risk abnormality (n = 182, 80%), and 2.6 years (1.7 - 3.1) for those with two cytogenetic high-risk abnormalities (n = 44, 20%). There were no patients with more than two cytogenetic high-risk abnormalities. Ninety-eight patients (45%) had a high-risk translocation, 77 (35%) had del(17p), 39 (18%) had a high-risk translocation plus del(17p), and 5 (2%) had gain(1q) plus either a high-risk translocation or del(17p). Figure 1 shows the Kaplan-Meier overall survival estimates stratified by the number of cytogenetic high-risk abnormalities (n = 226).
The presence of two cytogenetic high-risk abnormalities (compared to one) was of prognostic significance after adjusting for age, sex, and R-ISS stage (HR 2.01, 95% CI 1.27 - 3.19, p = 0.003, n = 205).
Conclusions: Approximately one in five patients with newly diagnosed high-risk multiple myeloma presented with two high-risk abnormalities at the time of diagnosis. These patients experienced inferior overall survival suggesting a cumulative effect of multiple cytogenetic high-risk abnormalities. The relatively low number of observed gain(1q) was likely related to the fact that not all patients were evaluated for that abnormality. Therefore the presented hazard ratio represents a conservative effect estimate and may underestimate the true effect.
Dispenzieri:GSK: Membership on an entity's Board of Directors or advisory committees; Jannsen: Research Funding; Alnylam: Research Funding; Celgene: Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Prothena: Membership on an entity's Board of Directors or advisory committees; pfizer: Research Funding. Kapoor:Takeda: Research Funding; Celgene: Research Funding; Amgen: Research Funding. Kumar:Janssen: Consultancy, Research Funding; BMS: Consultancy; AbbVie: Research Funding; Millennium: Consultancy, Research Funding; Onyx: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Sanofi: Consultancy, Research Funding; Skyline: Honoraria, Membership on an entity's Board of Directors or advisory committees; Array BioPharma: Consultancy, Research Funding; Noxxon Pharma: Consultancy, Research Funding; Kesios: Consultancy; Glycomimetics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal