Abstract
Background:Neural stem cell marker nestin is a suitable diagnostic and prognostic indicator of malignancy and potential cancer stem cells marker in solid tumors. Currently, nestin has been demonstrated as an epithelial-to-mesenchymal transition related protein associated with tumor metastasis, chemoresistance, and metabolic changes through altering mitochondrial dynamics in solid tumors. However its role in hematological malignancies remains unknown. Our recent work confirmed nestin protein as a tumor-specific marker for CD138+38+ plasma cells (PC) of multiple myeloma (MM) and potential predictor of worse response to conventional and novel therapy but prognostic potential of nestin has never been studied in MM so far.
Aim:The aim of this study was to evaluate whether pretreatment levels of nestin can predict overall (OS) and progression-free (PFS) survival of MM patients.
Methods: Nestin was detected in CD138+38+PC of 84 newly diagnosed MM patients (36M/48F; median age 70 years) by flow cytometry. Nestin was assessed as the percentage of nestin-positive PC (Nes+PC) and ratio of median fluorescence intensity of nestin (MFI ratio) and isotypic control. Survival cut-off points were established based on time-dependent ROC analysis. P-values below 0.05 were considered as statistically significant in all analyses. Cox proportional hazards models were used to assess the association of prognostic factors with OS and PFS. The independence of the marker was assessed by multivariate Cox regression model. Survival rates were estimated using the Kaplan-Meier method. Differences in survival among subgroups of patients were compared using the log-rank test.
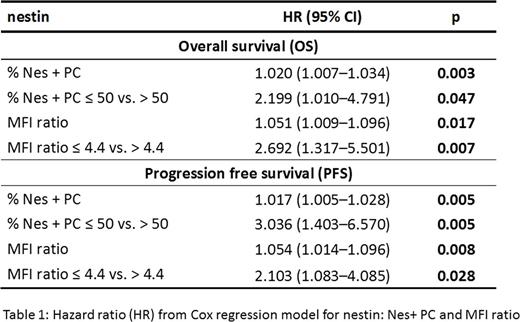
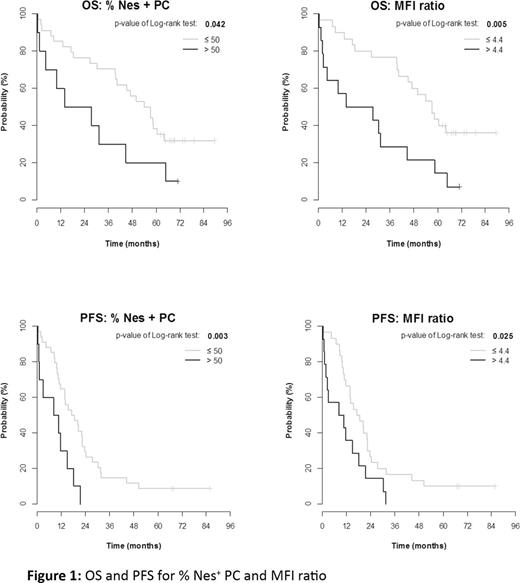
Results: ROC analysis divided patients into 2 groups: high (>50) and low (≤50) %Nes+PC subgroup and high (>4) and low (≤4) MFI subgroup. High %Nes+PC subgroup were associated with shorter OS (p=0.042) and PFS (p=0.003). High MFI ratio subgroup (>4.4) were significantly associated with shorter OS (p=0.005); and PFS (p=0.025) (Fig.1). Univariate hazard ratios (HR) showed prognostic impact of %Nes+PC (p=0.003) and of MFI ratio (p=0.017) for OS; %Nes+PC (p=0.005) and of MFI ratio (p=0.028) for PFS (Tab.1). 5 parameters: ISS: stage 3 vs. stage 1, del p53, age (at diagnosis), M protein type: IgG vs. other, LDH (µkat/l) and Beta2 microglobulin (mg/l) were significantly associated with OS after adjustment by nestin. However %Nes+PC or MFI ratio did not achieve independent prognostic status in multivariable model (p=0.223 and p=0.989).
Conclusion: These data demonstrate for the first time that nestin protein might have prognostic implication for MM. However, it does not appear to be independently associated with MM outcome when considering standard prognostic factors. The growing importance of nestin in key cell processes responsible for tumorigenesis and metastasis emphasizes the need for further investigation in MM. This pilot study requires to be further validated on a larger cohort of patients.
Supported by NT14575, RVO-FNOs/2014/17P, IRP201550, SGS03/LF/2015-2016.
Besse:Mundipharma-EDO: Other: travel support. Hájek:Takeda: Consultancy; BMS: Honoraria; Janssen: Honoraria; Amgen: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal