Abstract
Introduction:
Hypogammaglobulinemia is commonly observed in chronic lymphocytic leukemia (CLL), likely worsens over time and with chemoimmunotherapy, and eventually leads to infections which are a major cause of death in this disease. Unfortunately, newer therapies, such as ibrutinib, may not prevent the ongoing immunosuppression in CLL as a major cause of discontinuing this drug is increased infections. Nowadays, most patients present with early stage CLL, with an increasing number having monoclonal B cell lymphocytosis (MBL) and being followed for many years. CLL treatment is typically intensive, using chemoimmunotherapy with the therapeutic goal being to minimize tumor load. For these reasons, a reassessment of Ig levels in a CLL Clinic at diagnosis and during disease course in the 'real-life' setting has been carried out, along with an assessment of the need for Ig replacement.
Methods:
All CLL/SLL/MBL cases referred to the CLL clinic at CancerCare Manitoba, Winnipeg, Canada from 2007 to 2011 were included in this study. Immunoglobulin (Ig) levels (G, A, and M) were measured at the time of referral/diagnosis (baseline) and annually thereafter. Ig levels were correlated with patient characteristics (age at diagnosis, gender, comorbidities), CLL prognostic indicators (Rai stage, lymphocyte doubling time, creatinine, LDH, β2- microglobulin, IGHV mutational status, ZAP-70, CD38) and time to first treatment (TTFT). A subset analysis of patients treated with replacement gammaglobulin was also conducted.
Results:
There were 293 patents in this cohort with median age at diagnosis of 68 years. Of these, 62.5% were male, 38% had received treatment, and 24% died during the follow up time (median follow up of 71 months). Seventy percent of patients had CLL (of those 85% were diagnosed with Rai 0/I), 15% MBL and 15% SLL.
At baseline, 41% had normal Ig levels while 59% had a reduced level of one or more Ig (32% had reduced levels of one Ig type, 18% two, and 9% all three). Overall, 53% of patients had low IgM, 24% low IgG and 17% low IgA. However, no consistent correlation was found between the Ig levels at diagnosis and any of the prognostic markers outlined above.
Hypogammaglobulinemia (at least two consecutive values < normal) was associated with need for CLL treatment (HR 3.45, 95% CI 1.63-7.30, p=0.0012), while hypogammaglobinemia at diagnosis predicted a shorter TTFT (p=0.0008). Baseline IgA was also predictive of TTFT as well as overall survival, with patients with normal IgA having a longer TTFT, patients with high/low IgA a shorter TTFT (p=0.0012) and those with high IgA a shorter overall survival (p=0.0032). Furthermore, there was a positive correlation between baseline IgG and number of comorbidities (r=0.17, p = 0.0057) as measured by the Cumulative Index Rating Scale (CIRS) and β2-microglobulin levels.
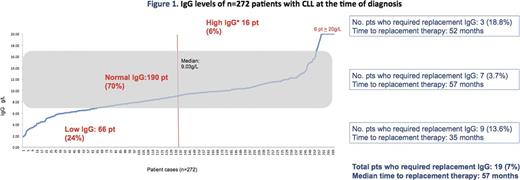
Eighteen patients (6.14%) required Ig replacement therapy, of those 13 (72%) were male and 13 (72%) had received chemotherapy. These patents also had a shorter overall survival than those not requiring IgG replacement therapy (p=0.0006). CLL cases with high baseline IgG are seven times more likely to require IgG replacement therapy (HR 6.92, 95% CI 1.78 - 29.91, p=0.0052) while cases with low baseline IgG are 5 times more likely (HR 4.99, 95% CI 1.59 - 9.43, p=0.0254) as compared to those with normal baseline IgG. Baseline IgA and IgM were not predictive of need for IgG replacement therapy.
Interestingly, over a median follow-up of 4 years, one-third of patients with normal baseline IgG developed a low IgG and this was unrelated to receiving chemotherapy (Figure 1).
Summary
This study demonstrates that baseline Ig levels in CLL are informative of the underlying biology of this disease, and could provide valuable information regarding disease progression, survival and need for subsequent IgG replacement therapy or CLL treatment. Importantly, Ig levels may be elevated in CLL and this is associated with increased CIRS and a high β2-microglobulin level, suggesting that the increase is related to underlying comorbidities. Further studies are required to examine the cause for the progressive decline in Ig levels over time, despite an otherwise stable disease, and to determine whether this decline can be eliminated by earlier treatment with novel new therapies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal