Abstract
Background and Aims: Myelodysplastic syndromes (MDS) are mainly diagnosed in the elderly with an increasing burden on healthcare systems. As a consequence, population-based studies are important in order to estimate the evolution of this emerging disease in different countries.
Objectives: The objective of this study was to provide trends ofannual case frequency, morphological subtypes, incidence, mortality and survival of patients diagnosed with MDS in Switzerland between 2001 and 2012.
Methods: A retrospective, population-based, epidemiological study was carried out on MDS cases reported to the Swiss Cantonal Cancer Registries and aggregated by the National Institute for Epidemiology and Cancer Registration. The Swiss Federal Statistical Office provided mid-year population estimates and cause of death statistics. Due to changes in the WHO classification of MDS, data was stratified for two time periods 2001-2007 and 2008-2012, respectively. 56 million person-years (py) were observed, covering 60%-65% of the Swiss population, during a time period of 12 years.
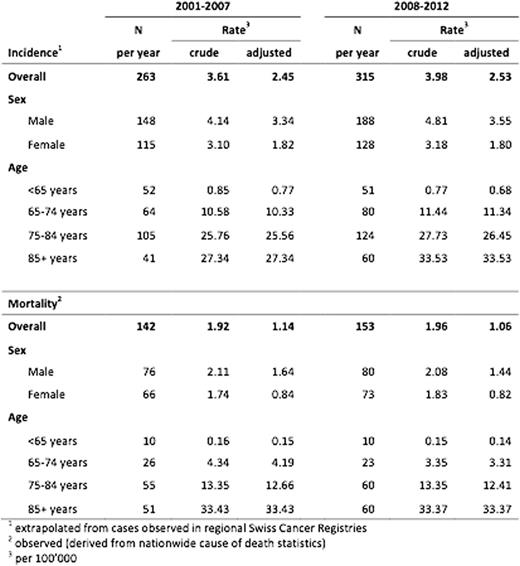
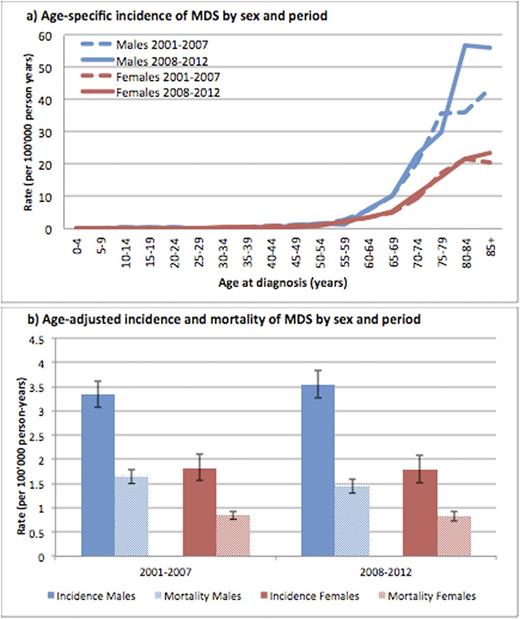
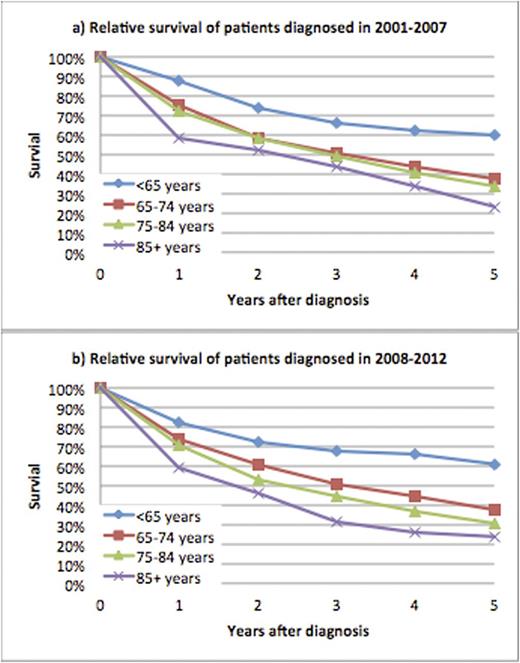
Results: 2138 MDS cases were reported with a median age of 77 years (range of means: 75-78 years). The estimated annual case frequency increased from 263 to 316 (+20%) but the overall age-standardized (adjusted) incidence-rate did not change between the time periods (Table 1). A substantial increase in incidence was only visible for men aged 80-84 (+57.7%), men aged 85+ (+29.3%) and women aged 85+ (+13.4%). With respect to mortality rates, a 10% decline was observed for men aged 85+. Incidence and mortality were very low below the age of 60 years but the rates steeply increased thereafter (Figure 1a). Irrespective of time period, incidence- and mortality-rates were almost twice as high among men compared to women (Figure 1b). Classification in MDS subtypes was poor and improved only modestly from 20% to 39% with a higher awareness for diagnosis of higher-risk diseases. Relative survival at 5 years (RS at 5y) for all patients was 37% in 2008-2012 with better survival for younger patients < 65 years (61%) compared to older patients > 65 years (24-37%). No differences in survival could be observed between the two time periods (Figure 2).
Conclusions: In this study we provide the first population-based, epidemiologic data from MDS patients in Switzerland. The analysis showed a 20% increase of annual incidence mainly due to population aging and not explained by increase in age-specific risk. This observation will impact on the future prevalence of the disease and its burden on healthcare systems.The age-specific incidence-ratesin patients > 75 years increased markedlyconsistent with the general increase of cancer-incidence in the elderly population. An increased diagnostic awareness of higher-risk disease seems to shift the population-based data for MDS sub-classification. We observed that younger patients without classified MDS subtypes have a similar survival like lower-risk disease, indicating that lower-risk MDS is underreported. Unsurprisingly, our data showed that younger patients have a better survival than elderly patients. This is most likelyrelated to higher frequency of lower-risk diseases in younger patients and their eligibility for allogeneic HSCT. However,the lack of a survival benefit observed in elderly patients on population-based level, after introduction of hypomethylating agents as standard treatment for transplant ineligible patients, is intriguing. The underlying reasons require further health-service research investigations.
Relevance: The currently available data from CCRs in Switzerland is insufficient for detailed health service research on MDS patients, since important data is lacking on treatment, side effects and outcomes. A new cancer registration law with mandatory notification of cancer cases will be implemented in Switzerland by 2018. Moreover, the Swiss MDS Study Group has launched a Swiss MDS Registry that has started recruitment in 2016. Both initiatives will be of great value to improve data collection in order to foster future health service research of MDS patients in Switzerland with international collaborators.
Incidence and Mortality of MDS in Switzerland in 2001-2007 and 2008-2012
Incidence and mortality of MDS in Switzerland in 2001-2007 and 2008-2012
Age-specific relative survival of MDS patients diagnosed in 2001-2007 and 2008-2012
Age-specific relative survival of MDS patients diagnosed in 2001-2007 and 2008-2012
Bonadies:Bristol-Myers Squibb: Consultancy; Celgene: Consultancy, Research Funding; Novartis: Consultancy, Research Funding. Ruefer:Novartis: Consultancy; Celgene: Consultancy, Research Funding. Gerber:Celgene: Consultancy. Benz:Celgene: Consultancy. Lehmann:Novartis: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal