Abstract
Myelodysplastic syndrome (MDS) is a heterogeneous group of hematopoietic stem cell disorders characterized by ineffective hematopoiesis and a high propensity to transform into acute myeloid leukemia (AML). Although hematopoietic stem cell transplantation can cure some MDS patients, most patients are not eligible to undergo the treatment because of advanced age or comorbidities. In order to choose the optimal treatments, predicting prognosis is crucial. Chromosomal karyotype, bone marrow (BM) blast percentage, and cytopenia are well-known prognostic factors for MDS patients. These factors are incorporated into the international prognostic scoring system and its revised version (IPSS-R). However, the impact of morphological abnormalities has not been fully determined. Thus, to elucidate this, we examined the influence of the number of dysplastic lineages and the presence of increased ring sideroblasts (RS) on the survival of MDS patients whose BM blast percentages were <5%.
Since 2006, the National Research Group on Idiopathic Bone Marrow Failure Syndromes, Japan, has been conducting the Prospective Registration, Central Review and Follow-up Study for Aplastic Anemia and Myelodysplastic Syndrome. Patients with BM blasts of <5% were subjected to our central review system for final diagnosis, and their medical records were collected every 6 months after their registration. By using this depository database, we retrospectively analyzed overall survival (OS) and cumulative incidence of progression to AML. This study was performed in accordance with the Declaration of Helsinki, and the study protocol was approved by the Ethics Committee of Kyoto University Graduate School and Faculty of Medicine and by the ethics committee of each participating institution. Either t test or Mann-Whitney U test was used as appropriate for analyzing the differences in variables between the groups. The Kaplan-Meier method and log-rank test were used for analyzing differences in OS between the groups. The Cox proportional hazards model was used for analyzing risk factors for OS, and Grayfs test was used for analyzing differences in cumulative incidence of progression to AML. P values of <0.05 was considered statistically significant.
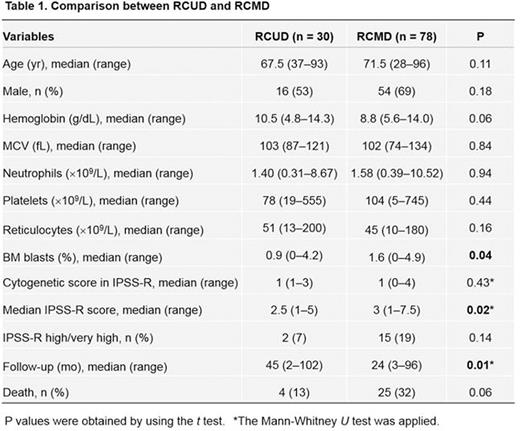
By May 2016, 351 cases had been registered to the depository. After central review, 216 cases were diagnosed as MDS according to definition by the French-American-British Cooperative Group. Cases that were not registered within 1 year after the time of institutional diagnosis and cases with follow-up periods of <4 weeks were excluded from this study. In the 2008 WHO classification, 30 cases were RCUD (MDS-SLD in the 2016 WHO classification) and 78 were RCMD (MDS-MLD in the 2016 WHO classification). The median ages of patients with RCUD and RCMD were 67.5 and 71.5 years, respectively (P = 0.11). The male-to-female ratios were 1.14 and 2.25, respectively (P = 0.18), and the median follow-up times of the survivors were 45 and 24 months, respectively (Table 1). Among patients with RCMD, 22 showed >15% RS in erythroblasts. The mean BM blast percentage was significantly lower in patients with RCUD than in those with RCMD, consistent with the result of our pervious study that used a different cohort where the BM blast percentages in patients with RA according to the 2008 WHO classification were significantly lower than those in patients with RCMD (Matsuda A, et al. Eur J Haematol. 2013;90:79-80). The 2-year OS of patients with RCUD was significantly higher than that of patients with RCMD (84% vs 76%, P = 0.014; Fig. 1a), which is consistent with the results of a German study (Maassen A, et al. Leuk Res. 2013;37:64-70). The cumulative incidence of progression to AML tended to be higher in RCMD than in RCUD, although the difference was not statistically significant (P = 0.0656, Fig. 1b). Among patients with RCMD, those with increased number of RSs showed significantly lower hemoglobin levels and higher cytogenetic scores according to the IPSS-R definition than those without increased RS (Table 2). The 2-year OS of the former was significantly inferior to that of the latter in our cohort (58% vs 87%, P = 0.009; Fig. 1c). Increased number of RSs is known to be associated with SF3B1 mutations, which in turn have been shown to be associated with favorable prognosis. However, the results of the present study indicate that in RCMD, an increase in the number of RSs may be an unfavorable indicator of patient survival.
Ozawa:Celgene Japan: Consultancy; Sumitomo Dainippon Pharma Co. Ltd: Research Funding; JCR Pharmaceutical Inc: Consultancy; Takara Bio Inc: Research Funding. Takaori-Kondo:Pfizer: Research Funding; Eisai: Research Funding; Takeda Pharmaceutical: Research Funding; Astellas Pharma: Research Funding; Kyowa Kirin: Research Funding; Cognano: Research Funding; Toyama Chemical: Research Funding; Mochida Pharmaceutical: Research Funding; Shionogi: Research Funding; Alexion Pharmaceuticals: Research Funding; Chugai Pharmaceutical: Research Funding; Janssen Pharmaceuticals: Speakers Bureau; Merck Sharp and Dohme: Speakers Bureau; Bristol-Myers Squibb: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal