Abstract

Background:
The presence of significant marrow fibrosis has previously been shown to be a poor prognostic factor in patients with myelodysplastic syndrome (MDS). Associations between fibrosis and higher transfusion requirements, multilineage dysplasia, and an increased rate of leukaemic transformation have been demonstrated. Currently, the presence of fibrosis is not included in standard risk scores for MDS such as the Revised International Prognostic Scoring System (IPSS-R) nor is fibrosis included in the current WHO classification for MDS. It is also not certain whether the presence of fibrosis should alter current treatment algorithms for patients. More information is needed to further assess both the prognostic and therapeutic implications of the presence of significant fibrosis in this patient population.
Methods:
We conducted a retrospective study utilizing a database of 247 patients with diagnosed MDS in a single center from 2000-2014. Bone marrow trephine samples for 200 of these patients were assessed using the European consensus on grading bone marrow fibrosis. Data was collected on: age, gender, WHO classification, marrow blast percentage, cytogenetics, progression to AML, treatment with azacitadine, and overall survival. These characteristics were compared between patients without significant fibrosis (grade 0/1) and those with significant fibrosis (grade 2/3). Our aim was to identify potential significant associations with MDS fibrosis and to assess whether treatment with azacitadine influenced these parameters or overall survival between the two groups.
Results:
Of 200 patients, 38 were found to have significant fibrosis (19%) versus 162 without significant fibrosis (81%).
There was no significant difference in age or gender between the two groups.
The commonest WHO category in both groups was RCMD (31.58% v 48.77%) in the fibrosis and non-fibrosis groups respectively. IPSS-R score was determined for 152 patients where data was available. There was no significant difference observed in IPSS-R Score between the two groups.
Cytogenetic data was available on 175 patients. The commonest cytogenetic result in both groups was normal karyotype (55.3% v 52.5%). In the fibrosis group this was followed by complex cytogenetics (> 2 abnormalities) (23.68%) and trisomy 8 (7.89%). The presence of a cytogenetic abnormality was not significantly different in those with or without fibrosis (p=0.69).
A significant difference was found between patients' marrow blast percentage at diagnosis (average 5.4% blasts in fibrotic patients versus 3.6% in non-fibrotic patients (p=0.04)). There were no differences in diagnostic haemoglobin level, neutrophil count, and platelet count.
Acute Myeloid Leukaemia (AML) developed in 31 patients. The presence of fibrosis was associated with an increased rate of AML transformation with 27% compared with 13.5% in patients without fibrosis (p=0.05).
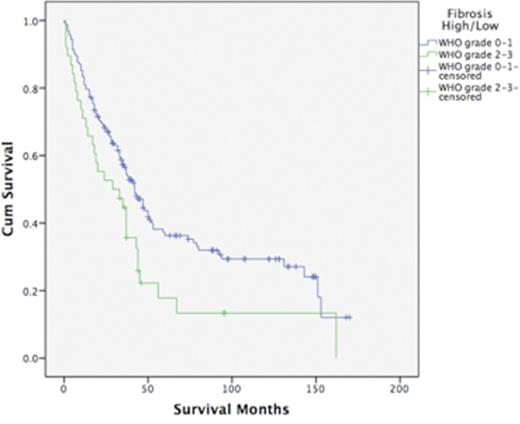
Median overall survival was decreased in the fibrosis group compared to the non-fibrosis group (29 months versus 42 months, p=0.02).
A total of 36 patients (25 of whom progressed to AML) received azacitadine treatment (9 (24%) patients with fibrosis and 27 (17%) patients without fibrosis). Patients with fibrosis had a longer median survival than those without (29 months and 19 months respectively) but this difference was not statistically significant (p=0.48).
Conclusion:
Marrow fibrosis adversely affects overall survival in patients with MDS. Patients with fibrosis are more likely to present with higher marrow blast counts and to progress to AML. Patients with fibrosis who received azacitadine appeared to have an overall higher survival than those without fibrosis. However, the numbers of patients who received azacitadine were small.
This study confirms the adverse prognostic influence of marrow fibrosis in patients with MDS, but the presence of fibrosis may not adversely affect the responsiveness to azacitadine therapy.
Desmond:Novartis: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal