Abstract
Background:
The myelodysplastic syndrome (MDS) includes a diverse group of clonal hematopoietic stem cell malignancies primarily affecting older individuals. It is characterized by bone marrow failure, peripheral blood cytopenias, and reduced survival. Treatment is based on prognostic scoring system and the pathology. Higher-risk disease carries a significant risk of progression to Acute Myelogenous Leukemia (AML). In these patients, treatment includes either an allogeneic stem cell transplantation (SCT) or a hypo-methylatingagent. Elderly patients with MDS usually are not a suitable candidate for allogeneic stem cell transplant given their age and other associated comorbidities. In this subset of patients, hypomethylatingagents, namely azacitidineor decitabineare the preferred treatment options. The effect of the introduction of therapeutic advances has not been well understood at the population level.We conducted this study to compare relative survival rates of elderly patients (≥65 years) with MDS in pre- and post- hypomethylatingagent era.
Methodology:
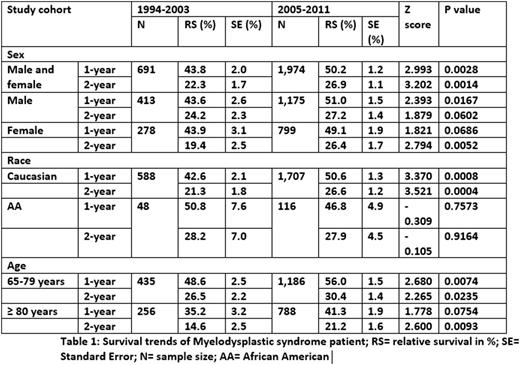
We utilized the National Cancer Institute (NCI) Surveillance, Epidemiology, and End Results (SEER-18) database to identify patients diagnosed with MDS. MDS subtype, namely Refractory anemia with excess blasts [Code: 9983/3] and Refractory anemia with excess blasts in transformation [Code: 9984/3] have the highest risk rate of transformation to AML. We opted to focus on these high risk MDS subtype. We limited our analysis to patients who are ≥ 65 years of age. On May 19, 2004, the U.S. Food and Drug Administration approvedazacitidinefor MDS. We defined our timeframes as follows: pre-hypomethylatingera (from 1994 to 2003) and post-hypomethylatingera (from 2005 to 2011). We analyzed one- and two-year relative survival rates (RS) of MDS patients. Several cohorts categorized by race (Caucasians and African Americans), gender and age (65-80, ≥ 80) were compared to assess the survival differences across our two defined eras. Z-test was used to compare the survival rates.
Results:
The database comprised of 2,665 patients (691 in pre and 1,974 in post). Overall there was an improved survival in post-hypomethylatingera (1-year: 43.8±2.0% vs. 50.2±1.2, Z-score= 2.993, p-value=0.0028; 2-year: 22.3±1.7 vs. 26.9±1.1, Z score= 3.202, p value=0.0014). There was a significant improvement in 1-year RS for males and 2-year RS for females. Elderly Caucasians also had survival benefit in post-hypomethylatingera. There was no survival benefit observed for African Americans however this did not reach statistical significance. A survival benefit was observed for elderly (65-79 years) and very elderly (≥ 80 years, only 2-year RS) population.
Conclusion:
The survival of myelodysplastic syndrome has improved significantly in post-hypomethylatingera. Improvements in supportive care, utilization of allogeneic stem cell transplant, andhypomethylatingagetnsmay all have contributed to this observation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal