Abstract
Background:
The Philadelphia chromosome negative chronic myeloproliferativeneoplasms (MPNs) including essential thrombocythemia (ET), polycythemia vera(PV), and myelofibrosis (MF) are a group of diseases of myeloid clonal lineage with significant symptom burden. MPN patients have also been found to have a high likelihood of mood disturbance related to their MPN, including symptoms of depression and anxiety (BMC Cancer. 201616:167). To date, the relationship between disease factors and depressive symptoms among MPN patients has not been well characterized.
Methods:
We have previously published the results of a 70-item internet-based survey which evaluated fatigue-relieving strategies among MPN patients (Cancer. 2016 Feb 1;122(3):477-85). Surveyed data included mental health questionnaires including a measure of symptoms of depression, the PHQ-2, (Ann Fam Med. 2010. 8(4): 348-353), a measure of positive and negative moods the POMS-short form (J Nerv Ment Dis. 1979;167(10):612-4) and a measure of symptoms of depression and anxiety, the MHI-5 (J Consult Clin Psychol. 1983. 51;730-742). This abstract is a secondary analysis of data collected among this cohort.
Data:
Demographics
A total of 1788 individuals diagnosed with an MPN participated in the survey. 1389 patients answered questions regarding mood and psychological comorbidities. Many MPN patients reportedthat they had been seen by a health provider for care or diagnosis of depression (32%), anxiety (29.5%), stress (26.2%), or grief(15.0%). Overall, 24.0% of ET, 22.2% of PV, and 22.9% of MF patients endorsed symptoms of depression based on their score of greater than or equal to 3 on the PHQ-2.
Demographic and Psychosocial Correlates
Younger patients were significantly more likely to have PHQ-2 score of equal to or greater than three (57.0 years vs 59.5 years, p=0.0006). Gender, race, and country of origin did not significantly correlate with screening positive for symptoms of depression. Higher BMI was associated with a higher likelihood of screening positive for symptoms of depression (BMI 26.2 vs 24.6, p=0.005). Not surprisingly, having received treatment for mood problems in the last 6 months (p<0.0001) along with medications for mood disorders (p=0.03) were significantly associated with increased symptoms of depression. Specifically, the use of psychostimulants (p<0.0001), antidepressants (p<0.0001), anti-anxiety medications (p=0.0005) and prescription pain medications (p<0.001), were significantly associated with elevated PHQ-2 score. Individuals with lower educational attainment were more likely to endorse depressive symptoms (p=0.0001) as well as those who were unable to work from home due to a medical disability (p<0.0001). Tobacco use was significantly associated with depressive symptoms (p=0.0002).
Symptom and Mental Health Correlates
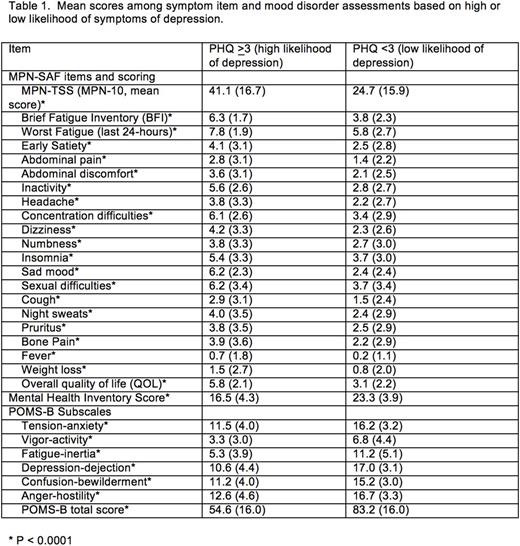
Increased MPN-SAF TSS (MPN-10) score and all individual symptom items in the MPN-SAF were significantly associated with symptoms of depression (p<0.0001, Table 1). Increased POMS-B Subscales scores and total score along with lower MHI score was associated with positive depression screening. When asking patients what interventions they had tried to reduce fatigue, those who endorsed volunteer activities (18% vs 25.4%, p= 0.0062) and exercise (19.7% vs 32.2, p<0.0001) were significantly less likely to screen positive for symptoms of depression.
Prognostic Risk Scoring Correlates
For MF, PV and ET prognostic risk scoring did not significantly correlate with PHQ score (for all, P>0.005).
Conclusions
Depression and mood disorders among individuals with malignancy represent a particular challenge for health care providers, particularly in MPN patients who have been found to have a higher risk of depression than the general population. In our cohort, prognostic risk did not correlate with risk of depression. Based on these findings, it is critical that physicians who see MPN patients should closely monitor these patients for signs of depression and provide appropriate treatment when needed. Continued investigation into treatment of mood disorders among MPN patients is warranted, as patients may benefit from both symptom-directed therapies as well as traditional therapies. Encouragement of volunteering and exercise activities should be considered for thesepatientsas participation may be associated with improved mood status.
Harrison:Novartis: Consultancy, Honoraria, Other: travel, accommodations, expenses, Research Funding, Speakers Bureau; Shire: Honoraria, Speakers Bureau; Gilead: Honoraria, Speakers Bureau; Baxaltra: Consultancy, Honoraria, Speakers Bureau; Incyte Corporation: Honoraria, Speakers Bureau. Mesa:Galena: Consultancy; Incyte: Research Funding; Gilead: Research Funding; Novartis: Consultancy; CTI: Research Funding; Promedior: Research Funding; Ariad: Consultancy; Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal