Abstract
Introduction. The characteristics of pathological clone cells in the Primary Myelofibrosis (PMF) strongly influence on the variability of the clinical course and prognosis. The main of them are type of driver mutation in JAK2, MPL or CALR genes ("clonal markers" (CM)), cytogenetic and epigenetic alterations. It is very important to provide the physicians necessary and sufficient information about the molecular profile of the disease to select the appropriate therapy for the patient.
The aim of our study was to investigate mutational diversity in PMF patients from the North-West region of the Russian Federation and to estimate overall survival (OS) depending on the type of CM, cytogenetic and epigenetic features.
Materials and methods. We examined 115 patients with PMF (45 male, 70 female). Median age was 59 years (range 19-82). The detection of V617F mutation of JAK2 was carried out for all the patients. JAK2(-) samples were tested for MPL gene 515 codon mutations and 9th exon mutations in the CALR gene. All patients underwent the analysis of mutations in EZH2, ASXL1 and IDH1 genes. Karyotype research was done for 47 patients with suitable bone marrow samples. Differences of mutation/karyotype occurrence in groups were assessed using the χ2 test. Survival curves were estimated by the method of Kaplan-Meier. Differences were considered as statistically significant with p-value <0.05.
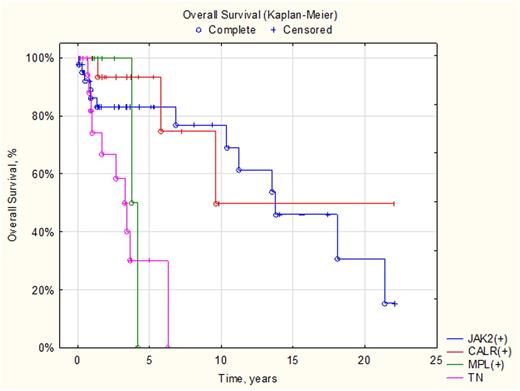
Results. CM were detected in 87 patients: JAK2(+) 47% (54/115), CALR(+) 23% (26/115), MPL(+) 6% (7/115) cases. No CM were found in 24% (28/115) patients, who considered as triple-negative (TN). The median survival of TN patients was significantly shorter than in the group of patients with any CM: 4 years vs 14.5 years, p=0.005. Five-year OS in TN patients was 30.6%, JAK2(+) - 83.8% and CALR(+) - 93.5% (p=0.046) (Figure 1). Median survival in JAK2(+) patients was 14.7 years, CALR(+) - 9.8 years. In MPL(+) patients with follow-up of 4 years median survival has not been reached.
Patients were divided into 2 groups based on the results of cytogenetic analysis: low-risk group (LR) included 27 patients with normal karyotype (NK) and 5 patients - with del(13)(q22), del(20)(q12), add(6)(p25), del(6)(q15) single features; high risk group (HR) consisted of 15 patients with complex abnormalities and unfavorable aberrations (+8, -7/7q-, i(17q), inv(3), -5/5q-, 12p-). Median survival in the LR group was 7.5 years, in the HR group - less than 1.5 years (p=0.025). Unfavorable karyotype frequency was distinct in groups with different CM: CALR(+) - 9.1% (1/11), JAK2(+) - 35% (7/20), TN - 54% (7/14), MPL(+) - 0% (0/2) cases but these differences were not significant (p=0.107).
We detected 28 mutations of the ASXL1 gene in 26/115 patients (22.6%): 24 patients had single mutation and two patients harbored two ASXL1 mutations at once. Mutation frequency was 13% (7/54) in JAK2(+) patients, 27% (7/26) in CALR(+), 32% in TN, 29% in MPL(+) (2/7). Differences in OS depending on the ASXL1-status were statistically significant in the TN group: median survival of the ASXL1(-) patients was 3.5 years, ASXL1(+) - 1.5 years (p=0.013).
Two mutations in the EZH2 gene (1.7%) were observed - each one in TN and ASXL1(+) patients. Both cases were characterized by rapid disease progression. The first patient (a 61-year-old male, complex karyotype) progressed rapidly to the blast phase from diagnosis and died after 8 months. The second patient (a 75-year-old male, NK) had severe thrombocytopenia and died from a hemorrhagic stroke 5 months from diagnosis.
We also detected 8 (7%) mutations in the IDH1 gene: 5 in CALR(+), 2 in TN, 1 in JAK2(+) patients. In seven cases it was a synonymous substitution G105 and in one case it was missense mutation R132C. The patient with the R132C mutation (a 74-year-old female, CALR(+), NK) had an unfavorable disease course: progression to blast phase was observed after 9 months from diagnosis. The patient died 13 months after disease progression.
Conclusion. CM and epigenetic mutations frequencies in our PMF patients is consistent with international data. Type of CM, cytogenetic aberrations and epigenetic changes can be correlated with different prognosis of PMF. The absence of any CM, unfavorable karyotype and ASXL1-status in TN patient are associated with reduced OS. The impact of ASXL1-status in patients with CM as well as EZH2 and IDH1-status on the prognosis in PMF patients requires further studies.
Shuvaev:Novartis pharma: Honoraria; BMS: Honoraria; Pfizer: Honoraria. Fominykh:BMS: Honoraria; Novartis Pharma: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal