Abstract
Introduction:
Primary cardiac lymphomas are rare non-Hodgkin lymphomas and account for less than 1% of intrinsic cardiac tumors and extranodal Non-Hodgkin lymphomas. Patients can present with a variety of manifestations including heart failure, chest pain, dyspnea, arrhythmias, and tamponade. Presently, there are no formal established guidelines for treatment of primary cardiac lymphomas.
Presentation:
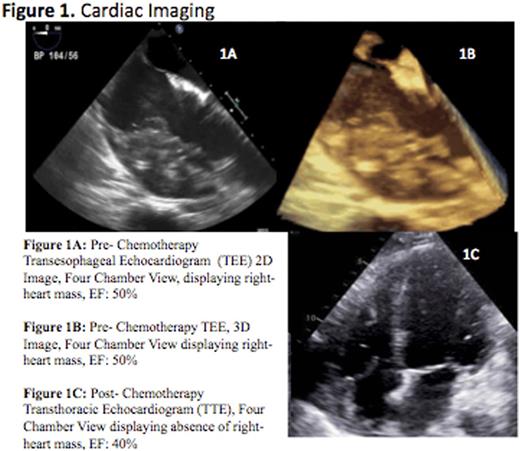
This is a case of a 72-year-old white man with past medical history significant for paroxysmal atrial fibrillation and known pulmonary, renal, and cutaneous sarcoidosis who presented with palpitations, dyspnea on exertion and lightheadedness for two-weeks. He was evaluated by his cardiologist who recommended an elective atrial fibrillation radiofrequency ablation (RFA). Prior to the planned procedure a transesophageal echocardiogram was performed which revealed a large tissue density within the pericardial space, adjacent to the free wall of the right ventricle and right atrium, and invading the myocardium with extension through the interatrial septum (Figure 1). The RFA was aborted and the patient was admitted for further evaluation of the new cardiac mass, initially suspected to be cardiac sarcoidosis.
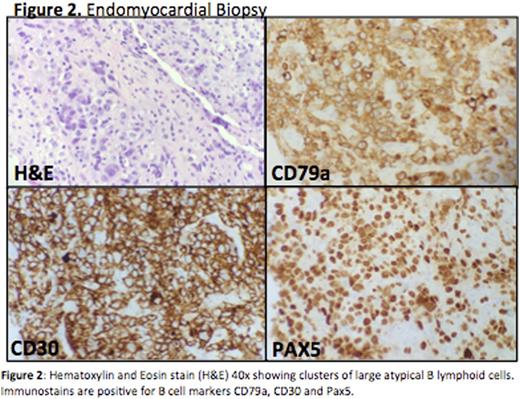
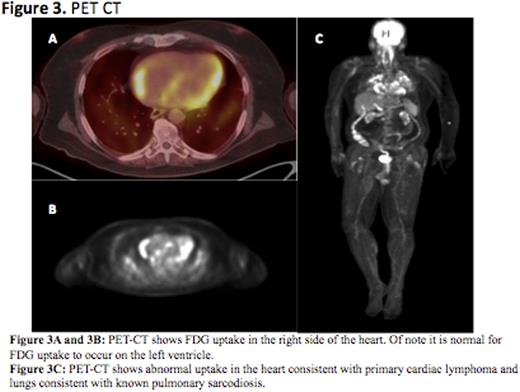
Subsequent work up included a cardiac MRI, which displayed a dense 7.5 cm by 3.5 cm mass involving the right ventricle and right atrium, wrapping around the great vessels. Right heart cardiac catheterization with endomyocardial biopsy was performed which revealed clusters of large atypical B lymphoid cells with the following immunophenotype: CD30+, CD79a+, Pax5+, Alk 1-, CD138-, CD 10-, Bcl 2-, Bcl 6-, CD45-, focally CD20+, Ki67: 80-90% (Figure 2). These findings were consistent with diffuse large B cell lymphoma (DLBCL). His PET-CT demonstrated absence of extracardiac lesions, confirming the diagnosis of primary cardiac lymphoma (PCL) (Figure 3).
The patient began treatment with a EPOCH-R (rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin) modified chemotherapy based regimen which consisted of a pre-phase treatment with dexamethasone 12 mg once daily for four days, a cumulative dose of cyclophosphamide 600 mg/m2 over five days and etoposide 50 mg/m2 for three days. Doses of cyclophosphamide and etoposide were initiated at lower doses and titrated upward to reach the target dose. This strategy was invoked based upon prior experiences and studies that suggest that a modest pre-phase cytoreduction reduces the risk of cardiac perforation. Rituximab was given on day six. He was also given granulocyte colony stimulating factor (GCSF).
Our patient was observed closely in the cardiac intensive care unit throughout the duration of chemotherapy due to the high risk of fatal arrhythmia, tamponade, perforation and heart failure. Interim restaging, confirmed complete remission of the intracardiac mass. His post chemotherapy TTE demonstrated a slight reduction in ejection fraction (Figure 1). He received a total of three cycles of EPOCH-R and remained hemodynamically stable within the hospital. No further chemotherapy was given due to a decline in the patient's performance status.
Conclusion:
This is the first documented case of primary cardiac diffuse large B cell lymphoma successfully treated with EPOCH-R consisting of a modest pre-phase cytoreduction with steroids, cyclophosphamide and etoposide. The high area under the curve of doxorubicin in this setting is far less cardiotoxic. This regimen reduces the risk of cardiac perforation in patients with relatively normal ejection fractions.
O'Connor:Mundipharma: Membership on an entity's Board of Directors or advisory committees; Seattle Genetics: Research Funding; TG Therapeutics: Research Funding; Bristol Myers Squibb: Research Funding; Spectrum: Research Funding; Celgene: Research Funding; Bristol Myers Squibb: Research Funding; Celgene: Research Funding; TG Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal