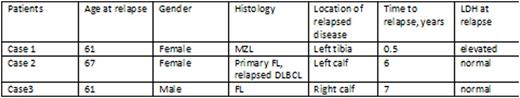
Background: While uncommon, non-Hodgkin's Lymphoma (NHL) can relapse in extranodal sites in the lower extremities. It is well established that venous thomboembolism occurs in higher incidence in patients with underlying malignancy. We describe 3 cases of NHL in which relapsed disease was discovered after lower extremity swelling prompted evaluation for deep vein thrombosis (DVT), and revealed recurrent NHL.
CASE 1: A 61 YO F with history of Stage IEA Marginal Zone Lymphoma (MZL) of the dura diagnosed in 2012 received treatment with whole-brain and local brain radiation. In 2016 she developed recurrence in cervical lymph nodes. Six months after receiving 4 cycles of bendamustine and rituximab she developed left leg pain and calf swelling. PET/CT showed a hypermetabolic lesion in left tibia. MRI confirmed large lesion in mid-shaft of tibia extending down the length of the bone. CT-guided bone biopsy confirmed MZL.
CASE 2: A 67 YO F with history of triple-negative inflammatory breast cancer treated in 2000 with neoadjuvant chemotherapy and mastectomy. PET/CT in 2008 showed 2 left femoral lesions. She underwent CT-guided bone biopsy of femoral lesion which confirmed follicular lymphoma (FL). Interim PET/CT in 2010 showed decreased FDG uptake in left femur. She was followed with watchful waiting. Then in 2014 patient developed leg swelling and pain, thought to be a DVT. Duplex ultrasound of the lower extremity was negative. PET/CT showed a left inguinal mass and left calf mass. MRI confirmed large mass within the left lower leg centered on the left fibular diaphysis with a very large associated soft tissue component with extensive muscular and neurovascular involvement. Biopsy of left inguinal lymph node confirmed diffuse large B-Cell lymphoma (DLBCL).
CASE 3: A 61 YO M with history Stage IV FL in 1988 and initially treated with 4 cycles of PROMACE-CytaBOM. He relapsed nodally in 1995 and was treated on the IDEC investigational protocol with rituximab which led to a complete remission. In 2001 he developed a subcutaneous nodule on his back, biopsy showed FL, grade 1. A staging CT scan of neck, chest, abdomen, and pelvis was unremarkable, but a PET scan showed left axillary disease. He was re-treated with rituximab and local radiation which led to a complete response. Patient presented in 2008 with right calf swelling. Ultrasound at that time showed no DVT but confirmed swelling and suggested right inguinal adenopathy. PET/CT showed FDG uptake in multiple areas in groin and pelvis plus extensive uptake in thickened calf muscles extending from the right knee to the toe. Biopsy of right inguinal lymph node confirmed FL.
Conclusion: Among NHLs, relapse patterns can vary significantly. Timing and frequency of relapse is largely dependent on whether NHL is classified as indolent or aggressive. However, location of relapsed disease in NHL is less well established. NHL relapse can occur in a fashion mimicking DVT with lower extremity swelling. When patients with history of NHL present with lower extremity swelling, relapsed disease should be included in the differential diagnosis.
Cohen:Takeda Oncology: Honoraria; Pharmacyclics: Honoraria; Seattle Genetics: Honoraria; Amgen: Honoraria. Broome:True North Therapeutics: Honoraria; Alexion Pharmaceuricals: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal