Abstract
Introduction
Acute lymphoblastic leukemia (ALL) is the most frequent cancer in childhood, but treatments' progress now allowsto obtain prolonged remission or curein over 90% of the patients. Consequently, therapeutic de-escalation is now an objective for future treatment protocols, providing that biomarkers allow to reliablyidentifygood responders. Among such indicators, low levels of Minimal Residual Disease (MRD) obtained early after induction chemotherapy stand out as good candidates. The latter can be investigated usingmultiparameterflow cytometry (MFC) or real-time polymerase chain reaction (RT-PCR) for immunoglobulins or T-cell receptors (IG TCR) rearrangements.
In this study we report the impact on survival of two early points of peripheral blood (PB) MRD assessment by MFC at days 8 and 15 on a cohort of 125 children with B-ALL enrolled in the French FRALLE trial and compared to molecular MRD in the bone marrow (BM) at day 35.
Patients and methods.
The study enrolled 67 boys and 58 girls and the duration of the study allowed for a median follow up of 52,1months. Median age at diagnosis was 57 months old (range 18 to 196), 101 children were between 1 to 10 years old and 24 were older than 10.
Complete blood counts (CBC) at diagnosis showed a median of 6.7x109/L leucocytes (range 0.47 - 151x109/L) and 33% blasts (range 0 to 97%). One hundred and eight children had less than 50x109/L leucocytes while 17 had higher counts. EGIL classification at diagnosis allowed to classify patients as three B-I, 94 B-II, 27 B-III and 1 B-IV. Cytogenetic analyses were performed for 118 patients who were partitioned as follows: low risk n=47, intermediate risk n=55 and high risk n=16 (Harrisson CJ et al., BJH, 2010). Eighty-three patients were in the low risk group and 42 in the high-risk group as described by the FRALLE protocol. Seven patients of the 64 tested had an IKZF1 deletion. During the duration of the study, 20 patients relapsed and 8 died.
Corticosensitivitywas defined by less than 1x109/L PB blasts on day 8 andchemosensitivity by less than 5% BM blasts on day 21 on BM smears.
PB MRD was assessed in MFC with a single five or ten colors tube adapted to each patient's leukemia associatedimmunophenotypeon a backbone of CD45, CD19, CD10 and CD38.
Statistical analyzes examined factors impacting disease-free survival (DFS) using Log rank test and Kaplan-Meier using theMedcalc® software (Ostend, Belgium). P values <0.05 were considered significant.
Results
None of diagnosis features had any significant impact on DFS: age (p=0,95), risk group (p=0,17), EGIL classification (p=0,55), cytogenetics (p= 0,87), leucocyte count (p=0,36) nor IKZF1 deletion (p=0,2). Of the 125 patients, 9 were corticoresistant, 79 corticosensitive and 37 not evaluable because of less than 1x109/L leucocyte at diagnosis.Corticosensitivity had no impact on DFS (p=0,11). Conversely,chemosensitivity had a significant positive impact on DFS (p= 0,009).
Day 8 PB MRD did not oultlineany significantly different DFS, whether considering detectable vs undetectable MRD (p=0.65) or MRD levels (logwisefrom >10-1 to <10-4, p=0,22).
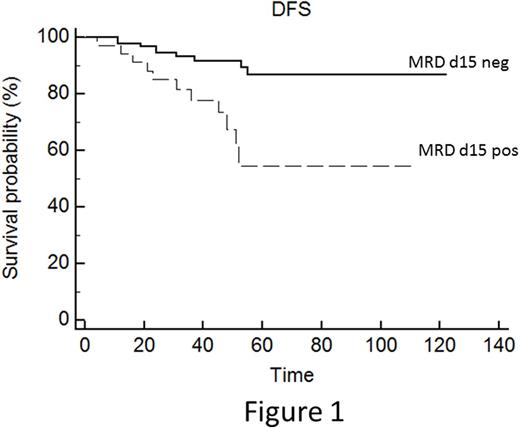
Conversely, PB MFC at day 15 appeared highly discriminant. Considering notdetectablevs detectable MRD, 4 years DFS was 91,6+3% vs. 67,6+9% p=0,0013 (Figure 1). Further refining the thresholds of MRD logwisedid not modify the significance (p=0.004; Figure 2). Indeed, DFS at 48 months was 61+15 % (n=16) for MRD >10-3, 74+11% ( n=18) for MRD <10-3->10-4 and 92+3% ( n=91) for MRD<10-4.
Comparison of PB MFC MRD on day 15 with day 35 BM molecular MRD showed concordance in 72% of the cases (83 negative/negative and 7 positive/positive, 48 months DFS 94.6+2.7% and 38+20% respectively). Eight patients were negative in PB but positive in BM (DFS 62.5+17%).Twenty seven where positive in PB but negative in BM (DFS 83.5+7.6%).These differences were statistically highly significant (p <0.0001).
Conclusion
This study demonstrates that even in the good prognosis context of childhood ALL, early MRD retains a highly significant prognostic value. It is of importance that this result was obtained not only on day 35 BM but interestingly, even earlier on day 15 PB. This less invasive procedure can easily be applied, especially for children. It should allow to detectgood responders, with MFC MRD levels below 10-4 for whom a de-escalation of chemotherapy could be considered. Conversely, the detection of blasts by MFC in day 15 PB is worrisome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal