Abstract
Background: The immune response is probably important for the long-term outcome of patients with tumours, including leukemias. However, its efficiency is often modulated by various immunosuppressive mechanisms, such as the expression of inhibitory receptors on the surface of the immune cells and of their ligands on tumor cells. The introduction of blocking antibodies against these receptors and ligands has gained considerable interest in the past several years and renewed the relevance of the stimulation of anti-tumor immune responses in the treatment of cancers. The significance of PD-1/PD-L1 expression in leukemias is not yet well established, although monoclonal antibodies targeting either PD-1 or PD-L1 are currently in clinical trials also for hematologic malignancies.
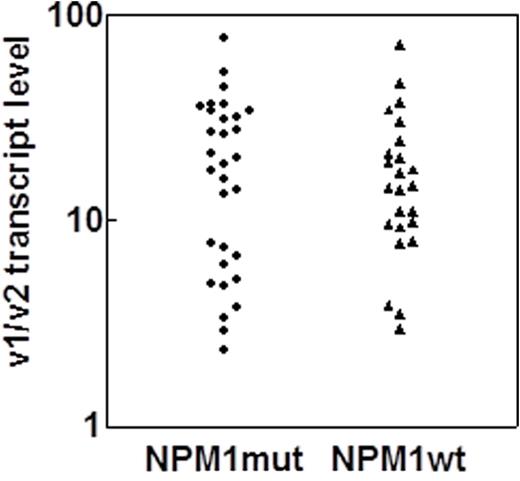
Aim and methods: We have recently shown that the surface expression of PD-L1 protein correlates with the ratio of two PD-L1 transcript variants (v1/v2) in hematopoietic cells (Brodská et al., submitted to Cancer Immunotherapy Research). This finding has enabled a retrospective examination of PD-L1 expression in frozen cDNA samples obtained from the peripheral blood of AML patients at diagnosis. A total of 55 patients with high leukocyte counts were selected for this analysis as their samples were presumed to be predominantly composed of leukemic cells. As our previous findings suggested the existence of anti-nucleophosmin immune response in vivo, the patients were divided into two groups according to the nucleophosmin mutation status.
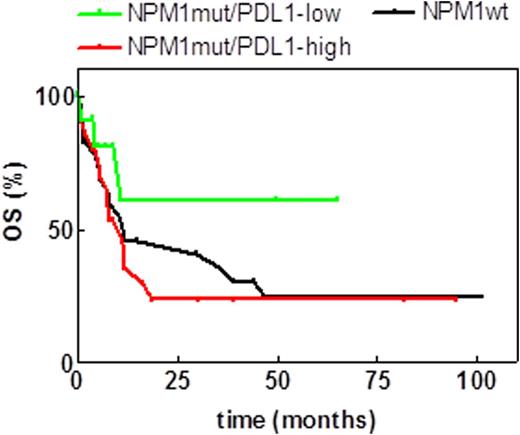
Results: The majority of the tested samples were PD-L1-positive (Fig. 1). The positivity was of 65% in patients with nucleophosmin mutations (NPM1mut, N = 31) and of 88% in patients with wild-type nucleophosmin (NPM1wt, N = 24). A better overall survival for PD-L1-low patients was observed in NPM1mut patient group, although the difference was not statistically significant (p = 0.21, Fig.2). The cutoff value for v1/v2 transcript levels was of 8.25.
Conclusions: Although PD-L1 expression in AML patients at diagnosis is usually low, we found very high incidence of PD-L1 positivity among patients with leukocytosis. Therefore, a high diagnostic leukocyte count may be associated with immune response failure in AML.
Acknowledgment: The work was supported by the Ministry of Health of the Czech Republic (grant No 16-30268A and the project for conceptual development of the research organization No 00023736).
PD-L1 expression in AML patients with high leukocyte counts at diagnosis. The surface expression of the protein was assessed through the ratio of the transcript levels for variants 1 and 2.
PD-L1 expression in AML patients with high leukocyte counts at diagnosis. The surface expression of the protein was assessed through the ratio of the transcript levels for variants 1 and 2.
Overall survival curves for AML patient groups according to PD-L1 expresssion and NPM1 status
Overall survival curves for AML patient groups according to PD-L1 expresssion and NPM1 status
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal