Abstract
Introduction/Background
Neonates are an intensively transfused group of vulnerable patients. Neonatal transfusion practice and general care has evolved over recent years, including the introduction of pedi-packs to limit donor exposure, and it remains important to audit practice. Inappropriate transfusions expose babies to potential adverse effects of transfusion. A national audit performed in the UK in 2010 concluded that there is a lack of evidence to back many of the existing recommendations for neonatal transfusion.
We undertook a prospective audit in order to review 5 years of transfusion practice in a tertiary NICU. Our current neonatal transfusion guidelines are based upon internationally published guidelines.
Aims & Objectives:
To determine the number of babies transfused, whether transfusions were adherent to local guidelines, to identify areas requiring improvement and to determine whether continuous auditing and feedback to clinicians improves practice
Methodology/Interventions This was a prospective audit conducted over a 5 year period. Data were prospectively and retrospectively retrieved from patient charts and electronic databases. Data were stored in a password-protected excel spreadsheet created on a secure hospital network.
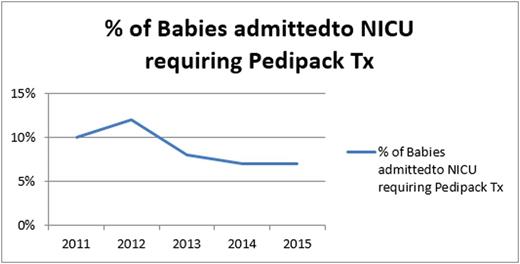
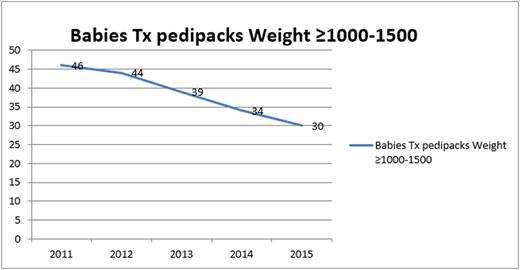
Results and Discussion A total of 557 babies were transfused with red cells during the period 2011 -2015, representing 7-12% of babies admitted to NICU. The median number of transfusions decreased in babies of all birth weight categories between 2011-2015. The biggest change was in babies <750g, where median donor exposure was reduced from 2 to 1 during this time. The overall percentage of babies admitted to NICU requiring a blood transfusion reduced from 12% to 7%. The most significant reduction was seen in babies ≥1500g with a reduction from 4% in 2011 to 2% in 2015.
Conclusions Auditing of neonatal transfusion especially in the area of pedi-pack top up transfusions highlighted specific areas where improvements could be made. This includes adherence to guidelines, consultant-led decision to transfuse (when time permits), and on-going audit and feedback to clinicians. These measures along with a multi-disciplinary approach to blood management have seen an overall reduction in percentage of babies being transfused without compromising the well-being of the baby. This has led to a reduction of donor exposure to the baby and a reduction in the cost and workload across all disciplines of staff associated with blood transfusion leading to an overall improvement to patient safety and quality of care. Despite this, the transfusion rate in babies of < 1000g remains the highest however this would be expected given the overall clinical needs of babies in this birth weight category.
Ní Áinle:Actelion UK: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal