Abstract
Specific aim: We have previously shown that platelets from patients with myocardial infarction (with ST elevation-STEMI) can activate T cells in vitro. In this study we wanted to expand our initial observation and explore the mechanism of this T cell activation.
Methods: After written informed consent was obtained, peripheral blood mononuclear cells (PBMCs) were isolated from heparinized venous blood obtained from 30 patients with STEMI (28 men and 2 women) at the time of hospital admission at diagnosis, before receiving any treatment, as well as 5 days and 30 days later. We also analyzed 15 healthy subjects (12 men and 3 women), and 7 patients with unstable angina who served as the disease control group. PBMCs were analyzed by flow cytometry with the following markers and their isotypic controls: CD4, CD25, CD127, FOXP3, and CD69. We also isolated platelet rich plasma or plasma alone from the patients and the healthy subjects, and used in mixed cultures with PBMCs. miR 155 levels were examined with real-time PCR.
Results: Initially, we incubated T cells with platelets from patients with STEMI and examined T cell activation by CD69 expression. These T cells showed increased expression of CD69 compared to T cells treated with platelets from healthy subjects (p<0.05). No T cell activation was observed following incubation with plasma alone from patients or healthy controls.
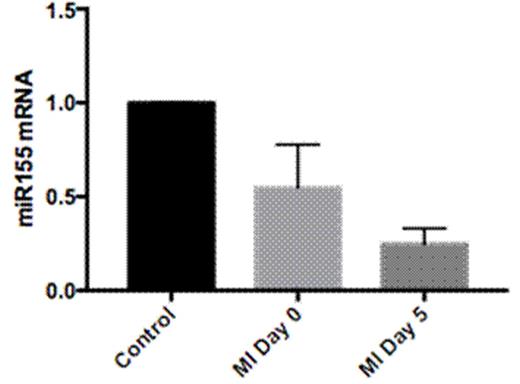
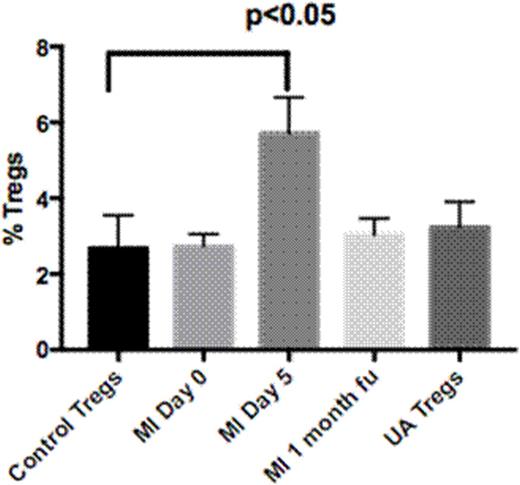
Next, the percentages of CD4+CD25+hi CD127low FOXP3+ (regulatory T cells, Tregs) were examined in all study subjects. Patients at presentation showed comparable Treg levels with the controls (healthy subjects and disease control group). Five days later, patients with STEMI displayed increased levels of Tregs compared with the controls (p<0.05) (Fig.2). To explore the mechanism of Treg up-regulation the miR155 levels through real time PCR were evaluated. Patients with STEMI showed comparable levels of miR155 at presentation, but five days later showed decreased miR155 levels compared to controls (p<0.001) (Fig. 1); we observed an inverse correlation between miR155 levels and Treg numbers in patients with STEMI. At re-evaluation, one month later, patients with STEMI displayed Treg numbers comparable to the initial presentation levels
Conclusion: Herein, we show that platelets from patients with STEMI can activate T cells in vitro. This platelet activation in patients with STEMI, results in an increase in Tregs through down-regulation of miR155, that return to normal levels a month later. This Treg increase reflects possibly an effort to suppress immune system activation secondary to platelet activation, shortly after the infarct.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal