Abstract
Introduction. Refractory autoimmune cytopenia may be a manifestation of an another underlying disorder like an autoimmune disease including the autoimmune lymphoproliferative syndrome (ALPS) or an immunodeficiency. Management of complex disorders of which cytopenia is only an epiphenomenon, could benefit of clinical and therapeutic approaches different from those applied to isolated autoimmune cytopenias.
Aim of the study. To design a scoring system to identify wider diseases underlying refractory autoimmune cytopenias and validate it on a patient population affected with this diseases referred to a national reference Pediatric Hematology Unit.
Patients and methods. Biochemical and clinical data on patients affected by refractory cytopenias were collected within the database of our Unit.after informed consent from the patients.
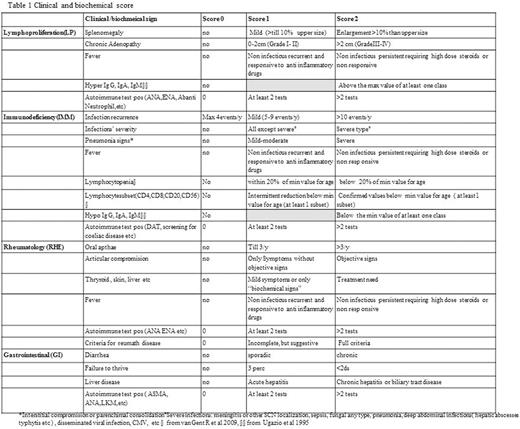
The symptoms/signs associated to cytopenia were arbitrarily grouped in 4 constellations: Lymphoprolypheration (LP), Immunodeficiency (IMM), Gastrointestinal (GI) and Reumathology (RHE). Each symptom/sign of the constellation was given a score (0, 1, 2 based on increasing the severity) whose sum constituted the final score of the single constellation (Table 1). If the score of each single constellation was up to 3, involvement was defined as mild. If the score was ≥4 the involvement was defined as severe.ALPS was defined according to NIH criteria.
Results. From 2000 to 2016, 78 patients (37males, 47%), median age 13.19 years (1.5-50.6 year) at last follow up, affected with refractory autoimmune cytopenia seen at our centre, were considered eligible for the study. In details: isolated cytopenia was shown in 60% of the cohort (Thrombocytopenia- ITP 72 % , Neutropenia-NP 19% and Autoimmune Haemolytic Anemia -AIHA in 12% of cases), bilinear cytopenia in 28% (ITP+NP in 64% of cases, AIHA +ITP in 27% and AIHA+ NP in 9% of cases) and trilinear cytoenia (AIHA+NP+ ITP) in 12% of the cohort.
In 85% of subjects cytopenia was associated to one or more constellation. In 77% of patients the association was with LP constellation; LP involvement was mild in 62% and severe in 38% of patients. In 69% of patients the association was positive for IMM constellation with mild and severe involvement in 70% and 30% of cases respectively. RHE constellation was positive in 58% (mild in 73% and severe in 27%) of patients. GI constellation was positive in 47% (mild in 89 % and severe in 11%). Patients positive for severe LP involvement were significantly associated to a diagnosis of ALPS (p=0.0003). ALPS was not associated with severe IMM constellation (p =ns). Patients with severe IMM score were significantly associated with severe RHE constellation (p=0.005). AIHA. either isolated or associated with other lineage cytopenia, was significantly associated with a severe IMM constellation (p=0.03).
Conclusions. About three quarters of patients with autoimmune refractory cytopenia had concomitant signs of lymphoproliferation or of immunodeficiency. Diagnosis of ALPS was significantly associated to severe LP but not with IMM whereas the diagnosis of AIHA was associated with severe IMM constellation. This scoring system looks as an helpful tool to drive underlying diagnoses, not only at very young ages, beyond refractory autoimmune cytopenias and therefore to orient appropriate diagnostic and management strategies of these patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal