Abstract
Background: First described in 2010, TAFRO syndrome is a clinical disorder presenting as thrombocytopenia, anasarca, fever, reticulin myelofibrosis, renal insufficiency, and organomegaly with unknown etiology. Onset of this syndrome is usually acute or subacute, and disease progression is rapid; a percentage of patients with this disorder have unfavorable clinical courses. Therefore, it is critical to identify an optimal management strategy for this disorder. Histopathological features of lymph nodes from patients with TAFRO syndrome are usually indistinguishable from that of patients with Castleman disease (CD) of mixed type histology. In addition, clinical features of patients with TAFRO syndrome are similar to those of patients with multicentric CD (MCD). Accordingly, some investigators assume TAFRO syndrome as a subcategory of idiopathic MCD (iMCD). However, whether TAFRO syndrome is entirely a part of iMCD category of diseases, or whether these are similar yet distinct disorders has not been clarified.
Aims: To elucidate the clinical features of TAFRO syndrome, and to clarify the association between TAFRO syndrome and iMCD.
Methods: Since 2013, a multicenter retrospective clinical study has been conducted by the Japanese TAFRO Syndrome Research Group. By July 2016, data of >200 patients with suspected TAFRO syndrome or MCD were collected. Utilizing this database, we compared laboratory data of patients with TAFRO syndrome with those of iMCD patients without TAFRO features. Diagnosis of TAFRO syndrome was defined according to our diagnostic criteria as previously described (Int J Hematol 2016;103:686-692), and the diagnosis of MCD was defined by pathological findings of lymph nodes. HIV or HHV-8 positive patients were excluded from this study. Comparisons between the two groups were performed using the Mann-Whitney U test. P values of <0.05 were considered statistically significant. This study was performed in accordance with the Declaration of Helsinki, and the study protocol was approved by the Ethics Committee of Kanazawa Medical University and by the ethics committee of each participating institution.
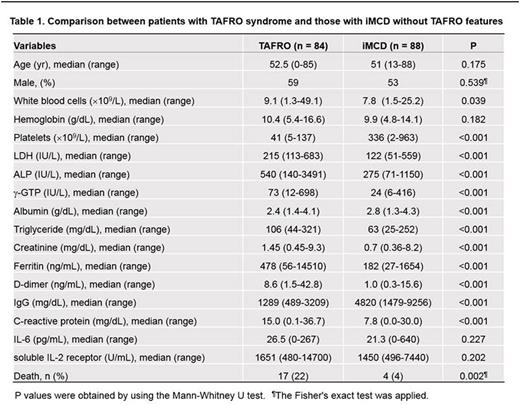
Results: According to our criteria, 84 patients were diagnosed with TAFRO syndrome, and 88 patients were diagnosed with non-TAFRO iMCD. Male to female ratios and median ages at diagnosis were comparable between these two groups. Hemoglobin, C-reactive protein, creatinine, lactate dehydrogenase (LDH), alkaline phosphatase (ALP), gamma-guanosine triphosphate (ƒÁ-GTP), ferritin, triglyceride, and D-dimer levels were significantly higher in patients with TAFRO syndrome than in patients with iMCD (Table 1). In contrast, platelet count, IgG, and albumin levels were significantly lower in patients with TAFRO syndrome than in patients with iMCD (Table 1). Seventeen of 84 TAFRO patients died due to disease progression, infection, or hemorrhage, whereas only 4 of 88 non-TAFRO iMCD patients died.
Discussion: TAFRO syndrome is defined based on clinical manifestations and CD is defined via typical histopathological findings of affected lymph nodes. Consistent with its definition, patients with TAFRO syndrome in our cohort showed low platelet counts and renal dysfunction, which were not commonly observed in non-TAFRO iMCD patients. Serum ALP and ƒÁ-GTP were significantly elevated in patients with TAFRO syndrome, whereas they were within the normal ranges in patients with non-TAFRO iMCD. Interestingly, serum IgG level was not elevated in TAFRO patients, whereas it was remarkably elevated in non-TAFRO iMCD patients. Similarly, low serum LDH level was another characteristic in iMCD patients that was not commonly observed in TAFRO patients. The majority of TAFRO patients showed D-dimer elevation, indicating that this syndrome is frequently accompanied by disseminated intravascular coagulation syndrome. Patients with TAFRO syndrome followed relatively aggressive courses, whereas most patients with non-TAFRO iMCD in our cohort followed indolent clinical courses.
Conclusions: Although several clinical and pathological features of TAFRO syndrome resembled those of iMCD, these two conditions manifested distinct laboratory parameters and differing clinical courses. From the results of this study, we postulate that TAFRO syndrome may not be a sub-category of iMCD and that both are distinct diseases with overlapping features.
Kinoshita:Zenyaku: Honoraria, Research Funding; Takeda: Research Funding; Chugai: Honoraria, Research Funding; Ono: Research Funding; Gilead: Research Funding; Eisai: Honoraria, Research Funding; Solasia: Research Funding; Janssen: Honoraria; Kyowa Kirin: Honoraria. Aoki:SymBio Pharmaceuticals: Consultancy. Masaki:Takeda: Research Funding; Kyowa Kirin: Research Funding; Chugai: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal