Abstract
Introduction: Patients with PNH often need surgery due to disease-related complications. However, surgery, anesthesia, and possible surgical complications, including inflammation and acidosis, can trigger complement activation, making surgery an important risk factor for hemolysis (Ando K, et al. Ann Hematol 2012;91:1987-8; van Bijnen ST, et al. Eur J Haematol 2011;87:376-8). Here we report data on the clinical management and treatment results of patients with PNH undergoing surgery.
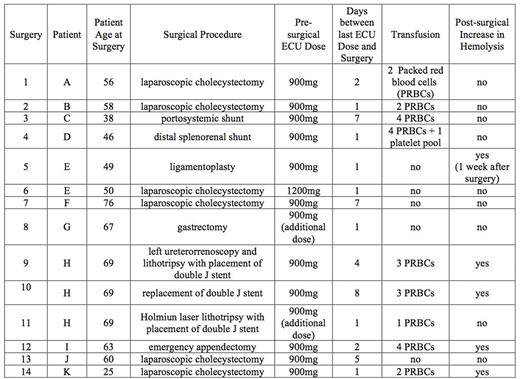
Patients and Methods: We collected data on 14 surgical interventions of 11 patients (8 males; age, 25-76 years). All patients had a high prevalence of PNH clone cells (55-99% in PMN) and were receiving eculizumab (ECU). Types of surgery were: 6 laparoscopic cholecystectomies, a transjugular intrahepatic portosystemic shunt, a distal splenorenal shunt, a laparoscopic Achilles allograft ligamentoplasty, a gastrectomy, an emergency appendectomy, and 3 urologic interventions. Ten patients received ECU 900 mg, while one (patient E, surgery 6) received 1200 mg since he had developed hemolysis at a previous surgical intervention (surgery 5). In two cases (patient G, surgery 8; patient H surgery 11), an additional dose of ECU was administered before surgery. Patient H (surgery 11) had developed hemolysis at previous surgical interventions (surgeries 9 and 10). In most cases, either the date of the ECU dose was taken into account when scheduling surgery or the ECU dose was moved forward to coincide with the date of surgery. The time between the last ECU dose and surgery was normally one day (range, 1-8).
Results: In nine cases, transfusions were required due to hemorrhagic complications. Patient I (surgery 12) had a thrombotic event leading to acute myocardial infarction one week after surgery. Increased hemolysis was observed (increased LDH and/or presence of hemoglobinuria) in five cases (patients E, H, I and K; surgeries 5, 9, 10, 12 and 14) during the week following surgery. Two of these patients (patients E and H) later underwent additional surgery (surgery 6, and surgeries 10 and 11, respectively). The pre-surgical ECU dose was increased in surgery 6 (patient E) and an extra dose was administrated in surgery 11 (patient H) and no hemolysis was observed. (See Table.)
Discussion: Our findings lead us to recommend that the date of surgery and/or the date of the ECU dose should be adapted to allow as short a time as possible between the last dose of ECU and surgery. Preferably, ECU should be administered just before surgery in order to avoid complications. The normal ECU dose could be increased or an extra dose be administered in order to minimize the risk of hemolysis in high-risk patients or in those with a previous history of surgery-related hemolysis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal