Abstract
Background: Improvements in multiple myeloma (MM) survival for patients diagnosed through mid-2000s have been well characterized; however, such improvements have not been shown among older patients and among racial/ethnic minorities. We hypothesized that the broader use of autologous hematopoietic stem cell transplantation introduced in the mid-1990s, and novel agents introduced since mid-2000s have further improved MM survival among all age and racial/ethnic groups.
Methods: We used data available from the Surveillance, Epidemiology and End Results (SEER-13) to calculate MM incidence and relative survival rates (RSR) for four time periods including 1993-1997, 1998-2002, 2003-2007 and 2008-2012. Follow up data were available through 2013. Data were obtained using SEER*Stat 8.3.2. Incidence and RSRs were calculated for non-Hispanic Whites (NHW), non-Hispanic Blacks (NHB) and Hispanics and for three age groups, <65, 65-74 and 75 years of age or older at time of diagnosis.
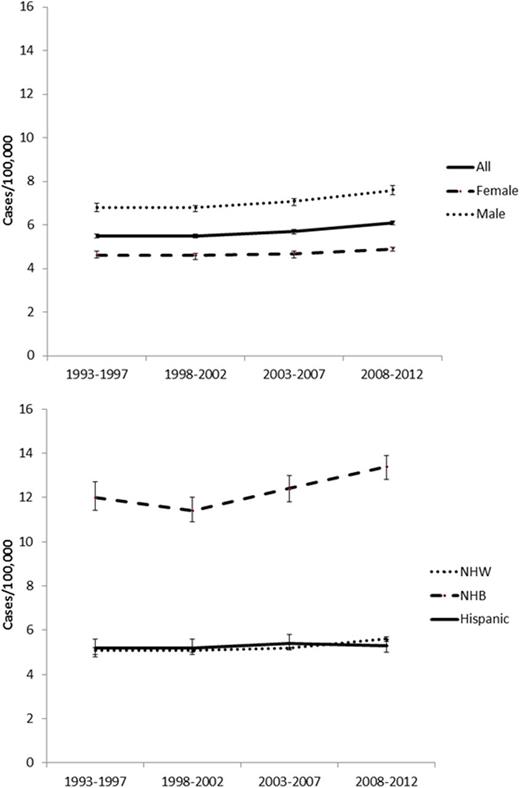
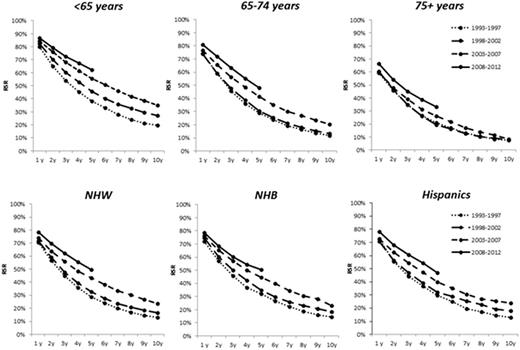
Results: We included a total 34,505 patients, of which n=7,494 patients were diagnosed between 1993-1997, n=7,952 patients between 1998-2002, n=8,803 patients between 2003-2007 and n=10,256 patients between 2008-2012. Overall, 13,229 (38.3%) patients were < 65 years of age, 9,834 (28.5%) 65-74 years of age, and 11,442 (33.2%) 75 years of age or older. There were 21,660 (62.8%) NHW, 6,349 (18.4%) NHB, and 3,599 (10.4%) Hispanic patients. MM incidence (per 100,000 persons) increased from 5.5 in 1993-1997 to 6.1 in 2008-2012 (P<0.001). An increase in incidence was observed among females (4.6 to 4.9, P<0.001), males (6.8 to 7.6, P<0.001), NHW (5.1 to 5.6, P<0.001), NHB (12.0 to 13.4, P<0.001), but not among Hispanics (5.2 to 5.3, P=0.7; Figure 1). Median age at diagnosis declined between 1993-199 and 2008-2012 from 72 to 69 years among females (P<0.001) and from 72 to 70 years among NHW (P=0.007), but not significantly among males (70 to 69; P=0.4), NHB (68 to 66 years, P= 0.4) or Hispanics (66 to 66 years, p= 0.9). RSR at 5 year (RSR-5), compared between 1993-1997 and 2008-2012 cohorts, improved among patients <65years (38.2% to 61.8%, P<0.001), 65-74 years (29.0% to 48.4%, P<0.001) and 75+ years (21.1% to 34.0%, P<0.001). RSR-5 improved among NHW (29.1% to 50.0%, P<0.001) at similar magnitude of the improvement among NHB (32.0% to 50.1%, P<0.001) and Hispanics (29.9% to 47.3%, P<0.001). RSR at 10 years (RSR-10), compared between 1993-1997 and 2003-2007 cohorts showed improvement among patients diagnosed <65 years (19.6% to 35.0%, P<0.001), and 65-74 (11.7% to 20.6%, P<0.001), but not among patients 75+ (7.8% to 9.3%, P=0.5). RSR-10 improved among NHW (13.2% to 24.3%, P<0.001), NHB (14.6% to 23.4%, P=0.002) and Hispanics (13.0% to 23.8%, P=0.001), Figure 2.
Conclusion: MM incidence has increased in recent years among NHWs and NHBs, but not in Hispanics. Improvements in RSR- 5 were evident for all age and racial/ethnic groups; however, improvements in RSR-10 were not detected for patients 75 years of age or older at diagnosis. The observed increase in MM incidence together with younger age of diagnosis and increased relative survival suggests a link between early intervention and prolonged survival.
Costa:Sanofi: Honoraria, Research Funding. Omel:Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Member of Takeda's "Patient Leadership Council". Token payment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal