Abstract
Continuous advancement in treatment strategies for childhood acute lymphoblastic leukemia (ALL) have improved survival rates markedly over the past decades. The overall 5-year survival rate is now approaches 90% for survivors treated with contemporary therapies that include central nervous system (CNS)-directed chemotherapy and intensified systemic chemotherapy. Late effects however, including neurocognitive deficits and osteonecrosis may present lifelong consequences for survivors. Children's Oncology Group (COG) protocol AALL0232 examined survival outcomes using a 2 x 2 factorial design that included randomizations for dexamethasone versus prednisone; and high dose methotrexate with leucovorin rescue versus escalating-dose methotrexate with PEG asparaginase. This study aims to describe the academic achievement and general adaptive functioning of patients treated on this protocol. We aim to identify demographic, clinical, and treatment factors that are associated with risk for adverse academic achievement and adaptive functional outcomes. We hypothesize that children diagnosed at younger ages (<10 years) will demonstrate more academic achievement difficulties than older children (≥ 10 years old). In patients ≥ 10 at diagnosis we hypothesize that older children will show evidence of greater adaptive difficulties. Additionally, we will explore differences between scores based on treatment regimen and insurance status.
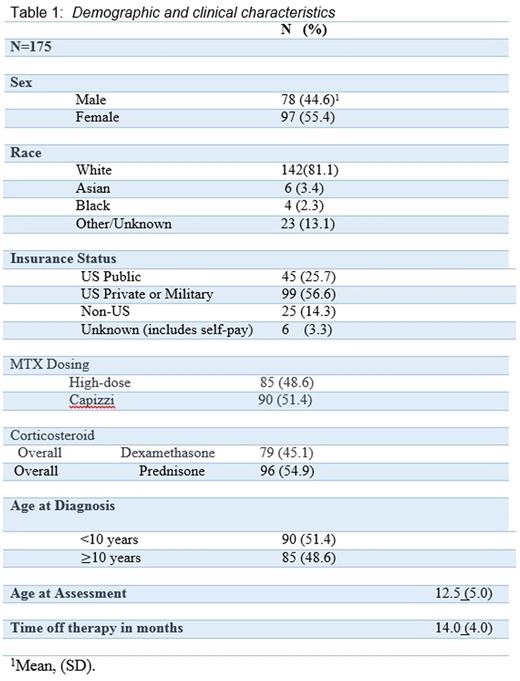
Methods: Patients with ALL, treated on COG AALL0232 protocol were identified and approached to participate on AALL06N1, a companion study designed to assess psychological outcomes. Of the 1386 children enrolled on the COG trial eligible for AALL06N1, general adaptive functioning data from 175 participants 8-24 months following completion of therapy were collected. Of these, 45.1% of the participants received dexamethasone and 54.9% prednisone; 48.6% received high dose MTX and 51.4% received escalating dose MTX. Participants were an average of 14.0 months off therapy, and had a mean age of 12.5 years (SD = 5.0 years) at the time of assessment. About 57% of participants had US Private or Military Insurance (Table 1).
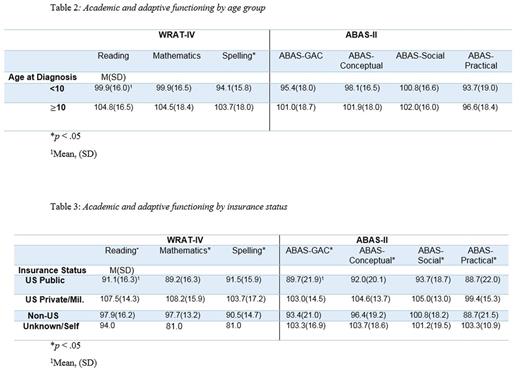
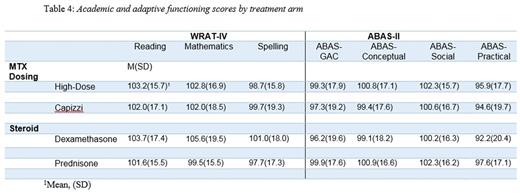
The Wide Range Achievement Test-IV (WRAT-IV; Wilkinson & Robertson, 2006) was used to assess academic achievement in reading, mathematics, and spelling. The Adaptive Behavior Assessment System II (ABAS-II; Harrison, 2003) is a parent-report measure of adaptive functioning. It results in three Adaptive Domain Scores (Conceptual, Social, Practical) and an overall General Adaptive Composite (GAC). All scores were age standardized.
Results: Mean scores for both academic achievement and adaptive functional outcomes were in the average range for all participants (Table 2). Younger children (< 10 years) performed more poorly on Spelling relative to older children (> 10 years). On general adaptive functioning, all mean scores were in the average range with no significant differences between age groups. Participants with private or military insurance had significantly higher academic achievement and adaptive functioning scores in comparison to public, non-US, and other insurances (Table 3). No significant differences were detected based on type of steroid or delivery of MTX (Table 4).
Discussion: On widely used measures of academic achievement and adaptive functioning, mean overall scores were in the average range among children treated for ALL. Consistent with a priori hypothesis, the observed academic achievement of younger children was slightly lower for reading and math than for older children, but was only significantly lower for spelling. Our second hypothesis was not supported as there were no significant differences between age groups on adaptive functioning. Participant scores were not dependent on treatment arm; however, insurance status was significantly associated with academic and adaptive functioning scores, particularly for participants with private/military insurance compared to the US public. These results suggest that academic achievement and adaptive functioning in survivors of childhood ALL are, on average, not different from population norms and remain in the average range, despite neurotoxic treatments. Future work needs to follow these trajectories longitudinally to ensure that more significant late effects do not emerge over time.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal