Abstract

Introduction: Venous thromboembolism (VTE) is the most common cause of hospital death. Pharmacologic intervention has become the standard of care in the prevention of VTE in hospitalized patients. However, studies have not been able to show a consistent benefit of VTE prophylaxis on mortality in hospitalized medical patients. Medical inpatients are a very heterogenous group; not all of them need VTE prophylaxis. Current guidelines recommend the use of heparin or related drugs as VTE prophylaxis in medical inpatients at increased risk of thrombosis, and recommends against pharmacologic VTE prophylaxis in patients at low risk. Several risk assessment modules including the Padua Prediction Score, attempt to identify patients at high-risk for thromboembolism. The goal of the study was to evaluate if risk is assessed and defined by clinicians prior to prescribing VTE prophylaxis.
Methods
A retrospective chart analysis was performed for patients admitted to the medicine service from January 2015 to June 2015. The initial arrival orders as well as the history and physical documented by the admitting physician were reviewed to determine if the risk of VTE was recorded and if VTE prophylaxis was prescribed. Patients were stratified as either admission or observation and the type of anticoagulation was recorded. If the admitting physician did not perform a VTE risk assessment, risk of VTE was calculated using the Padua Prediction Score.
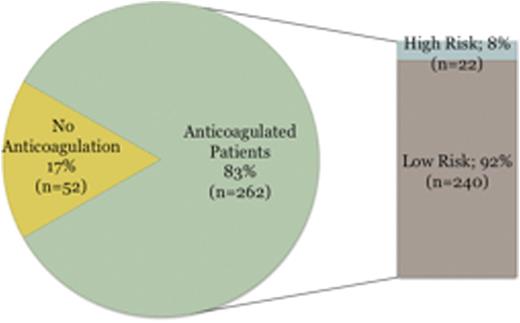
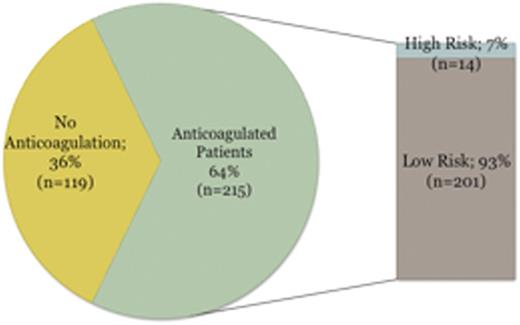
Results: Data was collected on a total of 648 patients. 314 (48%) patients met admission criteria and 334 (52%) patients met observation criteria. Chemical VTE prophylaxis was prescribed for 262 of the 314 (83%) admissions and 215 of the 334 (64%) observation patients. Of the 262 admissions that received chemical VTE prophylaxis, 240 (92%) of these patients were considered low-risk based on the Padua Prediction Score (Figure 1). 201 of the 215 (93%) observation patients that received chemical VTE prophylaxis were calculated to be low-risk (Figure 2). Adverse events were found to occur in 7 of the 648 (1.1%) patients that received chemical VTE prophylaxis.
Conclusion: Inappropriate use of chemical VTE prophylaxis was observed in a majority of medical inpatients.
Discussion: Routine use of VTE prophylaxis is not recommended. Current guidelines advise practitioners to evaluate all hospitalized patients for risk of VTE and bleeding prior to the initiation of VTE prophylaxis. Risk assessment tools such as the Padua Prediction Score help discriminate those patients at high risk of VTE and bleeding. However, this study shows that most clinicians do not perform a proper risk assessment for thromboembolism and bleeding prior to the initiation of VTE prophylaxis. Significant bleeding and thrombocytopenia were the most common complications identified in patients who received pharmacologic intervention. Although the rate of complications was low, further studies are needed to address additional negative consequences from the overuse of anticoagulation such as cost, nursing time and patient discomfort.
VTE risk assessment of anticoagulated patients who met admission criteria
VTE risk assessment of anticoagulated patients who met observation criteria
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal