Abstract
INTRODUCTION
There are many interventions in the disciplines of hemostasis and thrombosis that have been shown to be effective by high quality evidence, leading to the development of evidence-based guidelines by several professional groups. The extent to which providers and medical trainees make use of these guidelines in real-time clinical decision making is not known. Current hemostasis and thrombosis guidelines also lack an easy to navigate algorithmic design such as what is used by the National Comprehensive Cancer Network (NCCN) which may limit their utilization. Using several evidence based guidelines and consensus expert opinion we created an algorithmic tool designed to easily answer clinical questions in thrombosis and hemostasis, and conducted a prospective study assessing provider understanding of current evidence based recommendations and the effects of the algorithmic tool on clinical decision making.
METHODS
We implemented a prospective survey study of health care providers and medical students from the Oregon Health & Science University during July of 2016. Practitioners who care for patients with thrombotic or hemostatic issues were eligible; including internists, hematologist and oncologists, family medicine practitioners, nurse practitioners & physician assistants, hematology and oncology fellows, internal medicine and family medicine residents, and medical students. The survey included demographic questions, 11 clinical vignettes with multiple-choice questions asking participants for the most evidence-based treatment decision and to rate their confidence in the answer, and post-assessment feedback. Participants were encouraged to use the resources they would typically use in a clinical setting to make these decisions. Included subjects were randomly assigned access to our evidence-based algorithmic tool, (available online at http://tinyurl.com/Hemostasis-ThrombosisGuideline) available as downloadable PDF. The 11 clinical questions were scored, and an unpaired t-test was performed to determine if any significant difference existed in scores between participants with and without the evidence-based algorithmic tool.
RESULTS
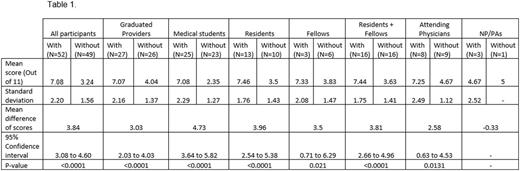
During the study period, 101 individuals participated: 48 medical students, 23 medicine residents, 17 attending physicians, 9 fellows, and 4 NP/PAs. Across all participants, those with access to the algorithms on average answered 3.84 (34%) more questions correctly (95% CI 3.08 - 4.60, P < 0.0001) (Table 1). Participants randomized to receive the algorithm were significantly more confident in their treatment decisions than participants without the algorithm (P < 0.0001). Significantly higher scores were found among individual groups including medical students, (mean difference 4.73, 95% CI 3.64 - 5.82, P < 0.0001), attending physicians (mean difference 2.58, 95% CI 0.63 - 4.53, P = 0.0131), and residents & fellows (mean difference 3.81, 95% CI 2.66 - 4.96, P < 0.0001). There was insufficient data to find a difference in score among NP/PAs who did and did not receive the algorithm. Participant reported confidence in their answers was significantly higher in those who were randomized to receive the algorithm (mean difference of0.95 on a 5-point confidence scale, 95% CI0.50 to 1.39, P < 0.0001).
CONCLUSION
Our study found that at baseline, there were limitations in provider and trainee understanding of the current evidence based management of clinical issues relevant to hemostasis and thrombosis, and that the use of an easy to navigate algorithmic tool significantly altered treatment decisions in commonly encountered clinical vignettes. Our findings suggest that utilization and decision-making may benefit from a more streamlined, algorithmic display of guidelines. Future prospective studies are needed to determine if such a tool improves management and outcomes in practice.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal