Abstract
Allogeneic HCT is a potentially curative but high risk therapy for patients with hematologic malignancies. HCT recipients are typically followed closely by their transplant center within the first 100 days, and with advances in supportive care, day 100 survival has continued to improve significantly over time. Longer term survival, however, remains a challenge and the factors that predict for later mortality are not well understood. We thus undertook this retrospective analysis to identify prognostic factors for 1-and 2-year survival among day 100 survivors.
Of 413 patients that underwent a first allogeneic HCT from 2006 to 2014, 355 survived >100 days post-transplant. Diagnoses included acute myeloid leukemia (N=163), myelodysplastic syndrome (N=89), acute lymphoblastic leukemia (N=62), chronic myeloid leukemia (N=34), or undifferentiated/biphenotypic leukemia (N=7). 34% of patients had high risk, 18% intermediate, and 48% low risk disease by American Society for Blood and Marrow Transplantation (ASBMT) RFI risk category. Median age at transplant was 50 years (range, 18-73). The majority of patients were Caucasian (89.6%). Median household income was $49,980 (range 13,316-112,530) and median distance from transplant center was 46 miles (range, 1-1055). 40% patients had a high HCT co-morbidity index, 32% intermediate and 28% low. 152 (43%) patients underwent a matched related donor, 148 (42%) matched unrelated donor, 36 (10%) umbilical cord blood (UCB), 13 (3%) haplo-identical, and 6 (2%) mismatched unrelated donor transplants. The majority of patients (75%) underwent a myeloablative transplant and bone marrow (BM) (53%) was the primary graft source.
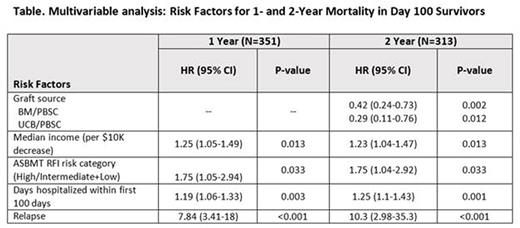
Cox proportional hazards was used to identify prognostic variables for 1- and 2-year mortality in the 355 surviving patients using baseline characteristics and factors evaluated at day 100. Baseline characteristics as described above included patient, disease, transplant, and socioeconomic/psychosocial factors. Additional variables evaluated at day 100 included number of readmissions, days hospitalized, GVHD rates, infections, relapse within the first 100 days of transplant, and QOL measures as assessed by the Functional Assessment of Cancer Therapy Bone Marrow Transplantation (FACT-BMT), scored at baseline and day 100.
1- and 2-year mortality was 71%, and 54%, respectively, compared to a day 100 mortality of 86%. Among day 100 survivors, the most common causes of death within the first 2 years were relapse (N=78, 54%), followed by infection (N=24, 17%), pulmonary or other organ failure (N=23, 16%), and GVHD (N=16, 11%). In multivariable analysis evaluating risk factors for mortality among the day 100 survivors, lower income (HR 1.25, P=0.013), high risk ASBMT RFI (HR 1.75, P=0.03), relapse (HR 7.84, P<0.001), and more days hospitalized within the first 100 days (HR 1.19, P=0.003), were associated with increased mortality at 1 year (Table). Similar risk factors were identified for 2-year mortality, however, patients receiving BM and UCB grafts had lower mortality long-term as well.
In summary, although relapse remains the biggest cause of treatment failure and mortality after allogeneic HCT, we also highlight findings that increased hospitalization within the first 100 days and low socioeconomic status is associated with worse long-term survival. While early post-transplant care is typically well-coordinated through the transplant center, our findings suggest that patients who may have had complications within the first 100 days and survivors with lower socioeconomic status and potential poor access to healthcare may be at higher risk for longer term complications. Further studies are needed to identify these at-risk, resource limited patients that may benefit from longer and closer follow up or additional interventions to improve long-term post-HCT care and non-relapse mortality.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal