Abstract
INTRODUCTION:
High-dose chemotherapy and autologous hematopoietic stem cell transplantation (auto-HCT) is the standard of care for eligible patients with newly diagnosed multiple myeloma. However, almost all patients eventually relapse possibly due to incomplete elimination of malignant plasma cells. For patients with an identical twin, syngeneic-HCT provides a tumor-free graft without the risk of graft vs. host disease. We hypothesized that syngeneic-HCT would result in better disease control than auto-HCT.
METHODS:
We identified 10 patients with multiple myeloma who underwent syngeneic-HCT at our institution from 1994 to 2014. Using a propensity score, we identified 48 controls that received auto-HCT during the same time interval. Matching was done for the year of transplant, age and disease status at auto-HCT (Table 1). Primary endpoint was progression-free survival (PFS). Secondary endpoints were complete remission (CR) rates and overall survival (OS).
RESULTS:
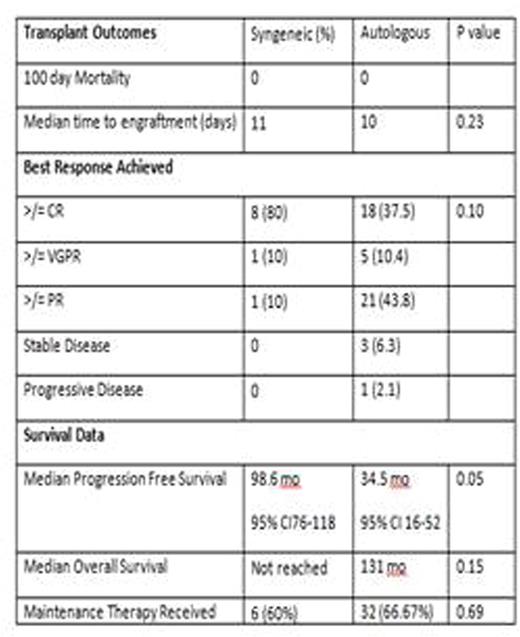
Baseline characteristics are shown in Table 1. The two groups were well matched, with no significant statistical differences in age, sex, race, stage at diagnosis, lines of therapy received, or disease status prior to transplant. At the time of transplant, 7 (70%) patients in the syngeneic cohort were in first remission, with 3 (30%) having relapsed disease. Similarly, 28 (58%) patients in the autologous cohort were in first remission, with 20 (41%) having relapsed disease (p value 0.49). Patient outcomes are summarized in Table 2. All patients engrafted, with a median time to engraftment of 11 and 10 days, for the syngeneic and auto-HCT cohorts respectively (p=0.22). There was no treatment related mortality in the first 100 days post-transplant in either of the cohorts. In the syngeneic group 8 (80%) patients achieved ≥ CR, 1 achieved very good partial remission (VGPR), and 1 achieved a partial remission (PR), with an overall response rate (ORR) of 100%. Amongst the control group, 18 (37%) achieved ≥ CR, 5 (10%) achieved ≥ VGPR, 21 (43%) achieved ≥PR, 3 (6%) had stable disease and 1 (2%) had disease progression, with an ORR of 91.6%. There was no significant difference in the ORR between the two groups (p=0.21). At the time of last follow-up, a total of 4 (40%) patients had relapsed in the syngeneic cohort, and 31 (65%) had relapsed in the autologous cohort (p=0.15). The median progression free survival (PFS) for the syngeneic cohort was 98.6 months (95% CI from 76-118 months), while the median PFS for auto-HCT cohort was 34.5 months (95% CI from 16-52 months) (p=0.05). Median overall survival (OS) for the syngeneic and auto-HCT cohorts were not reached and 131 months, respectively (p=0.15). The PFS difference was not due to a difference in maintenance therapy after transplant, as 6 (60%) syngeneic patients and 32 (66.7%) auto-HCT (p=0.69) received maintenance therapy respectively.
CONCLUSION:
Our study shows that patients with multiple myeloma who underwent syngeneic-HCT had a trend to a higher CR rate and longer PFS compared to a matched cohort that underwent auto-HCT. This benefit may be related to the absence of malignant plasma cells in the syngeneic graft, and a normal donor immune system. The efficacy of syngeneic transplants needs to be assessed in a larger number of patients to provide sufficient power to detect clinically meaningful differences with autologous transplants.
Kaplan Maier Curves for Progression Free Survival and Overall Survival.
Kaplan Maier Curves for Progression Free Survival and Overall Survival.
Bashir:Takeda: Consultancy; Spectrum: Consultancy; Takeda: Research Funding; Celgene: Research Funding. Champlin:Ziopharm Oncology: Equity Ownership, Patents & Royalties; Intrexon: Equity Ownership, Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal