Abstract
Introduction: Fertility preservation is crucial in the setting of hematopoietic stem cell transplantation (HSCT) due to the severe impact of infertility on quality of life in long term survivors. Many chemotherapy agents as well as CNS or pelvic irradiation can affect gonads leading to impairment of pubertal development and/or infertility. In the last years different fertility preservation guidelines especially for cancer patients have been published. Despite these recommendations options for fertility preservation are not well established in children, it's discussed only in about 42% (Terenziani et al. PBC 2014) of all eligible patients. We present here a survey conducted by the Pediatric WP of the EBMT.
Aim: to analyze and compare the different fertility preservation practices for children and adolescents across the EBMT centers and to identify hence the unmet needs in the field.
Material and Methods: The survey was conducted between September 2014 and December 2015. 177 pediatric centers reporting to the EBMT were asked to fill-out a form with 24 questions related to fertility preservation strategies. Questions focused on institutional availability of a fertility preservation program and its options, number of patients included in the program, payers and suggestions for improvement.
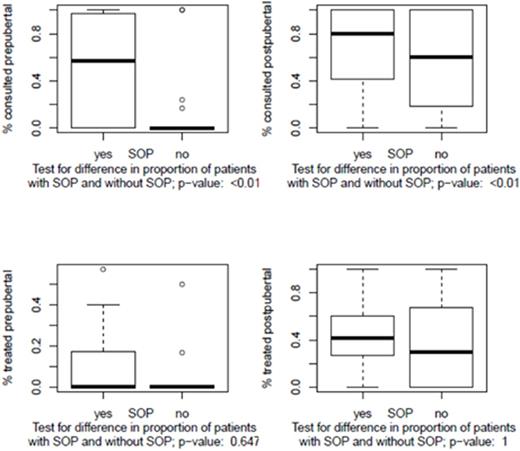
Results: 38 (21%) centers from 16 countries replied. In 2013 the number of HSCT per center ranges from 2 to 60. Totally, 834 children were transplanted in the 38 centers, 22% of the reported HSCT in children (3789) in 2013 from the EBMT centers. Of the 834 patients 612 (73%) were prepubertal and 203 (25%) postpubertal. 322/834 (39%) patients received a fertility preservation counselling and 243 (29%) of them had a fertility preservation procedure. Half of the 38 centers reported to have a fertility preservation program with standard operating procedure (SOP) for counselling. Centers with SOP counselled patients significantly more often than those without (Figure 1A). Regarding the number of applied procedures, no significant difference was found between centers with and without a SOP (Figure 1B). Centers with SOP counselled earlier (at the beginning of treatment/diagnosis; 61% versus 29%), and an interdisciplinary counselling team was largely used (60%). This team involved hematologists, gynecologists and /or reproductive medicine specialists. The most frequently cited reasons for missing counselling were lack of time (59%), refusal by parents (35%) and expected poor prognosis (29%). Reasons explaining parents/patients refusal were psychological distress (52%) and overwhelming feeling (50%) in this life-threatening moment. All responding centers considered the topic of fertility preservation as very relevant. Better education, more resources and financial funding emerged as pivotal factors to support and implement such programs.
Conclusion: This EBMT survey showed the great interest for fertility preservation in participating centers. The collected data indicated that less than half of pediatric and adolescent patients undergoing HSCT in 2013 received a counselling on fertility preservation and/ or underwent fertility preservation procedures. This emphasizes the need for enhanced education of the transplant team and active multidisciplinary collaboration in the field. Fertility preservation becomes a standard of care; this data represents the basis to further efforts toward fertility preservation standardization in the EBMT community.
Upper figures: Percentage of consulted patients in centers with and without SOP. Lower figures: Percentage of treated patients in centers with and without SOP
Upper figures: Percentage of consulted patients in centers with and without SOP. Lower figures: Percentage of treated patients in centers with and without SOP
Bader:Servier: Consultancy, Honoraria; Neovii Biotech: Research Funding; Riemser: Research Funding; Medac: Consultancy, Research Funding; Novartis: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal