Abstract
Background: In utero hematopoietic cell transplantation (IUHCT) results in long-term, multilineage chimerism without myeloablation/immunosuppression. It has the potential to treat a number of congenital hematologic disorders, including as Sickle cell disease. Central tolerance, through which donor-reactive host T cells and host-reactive donor T cells are deleted, is instrumental to the induction of donor specific tolerance (DST) and the prevention of graft-versus-host-disease (GVHD). Central deletion, however, is incomplete, and donor-reactive host T cells remain following allogeneic IUHCT. Furthermore, central deletion alone cannot explain the absence of GVHD either following IUHCT using non-T cell depleted bone marrow (BM) or in chimeric animals that undergo postnatal donor lymphocyte infusion (DLI) with subsequent conversion to >90% allogeneic donor cell engraftment (Hayashi et al., Blood 2002;100:804-12). Studies in both mice and humans have demonstrated the importance of regulatory T cells, including traditional CD25+FoxP3+ Tregs and CD49b+LAG-3+ Type 1 regulatory T (Tr1) cells, in maintaining tolerance following postnatal allogeneic transplantation. We hypothesized that peripheral regulatory T cells are increased in chimeric animals following IUHCT and that they contribute to the establishment of DST and prevention of GVHD.
Methods: 10x106 BM cells from 6-8 week old C57Bl/6 (B6) FoxP3GFP mice (H2Kb, CD45.2+) were injected intravenously (IV) into gestational day 14 Balb/c FoxP3GFP fetal recipients (H2Kd, CD45.2+). Mice were sacrificed at 2, 4, 8, and 24 weeks of age. Splenocytes were analyzed for the expression of CD4, H2Kb, H2Kd, CD49b, LAG-3, CD25, and FoxP3 to determine the percentage of traditional Tregs and Tr1 cells within the CD4+ population as well as for the expression of intracellular IL-10 - a key mediator of regulatory T cell function. A GVHD model was developed in which 10x106 B6 BM cells were injected IV into day of life 0 (P0) naive Balb/c mice. The ability of IUHCT-induced regulatory T cells to suppress GVHD was assessed in two groups: 1) 10x106 B6 BM cells injected into P0 mice that had undergone IUHCT and 2) 10x106 B6 BM cells co-injected with 5x106 CD4+ splenocytes harvested from 2 week old chimeric mice into P0 naive Balb/c mice. To evaluate the role of regulatory T cells following DLI in chimeric mice, 30x106 B6CD45.1 (H2Kb, CD45.1+) splenocytes were injected IV into 4 week old chimeric recipients. Mice were sacrificed at 48 hours and 2 weeks post-DLI, and regulatory T cells were measured as a percentage of CD45.2+CD4+ cells in the spleen.
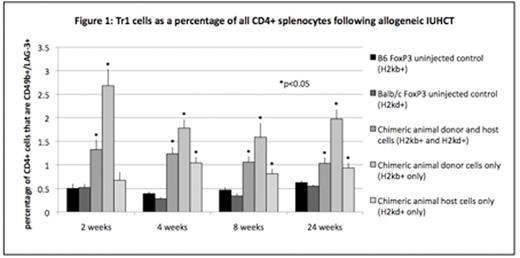
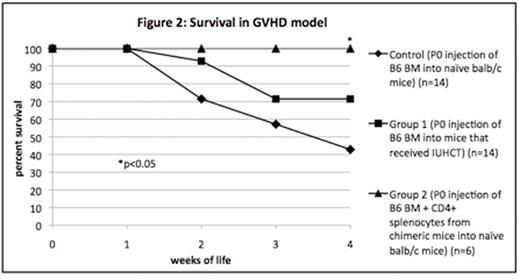
Results: IUHCT was associated with a significant increase in Tr1 cells, predominantly of donor origin, compared to naive controls (Figure 1). There was a corresponding increase in intracellular IL-10 expression in donor CD4+ splenocytes in chimeric animals compared to naive B6 FoxP3GFP controls at 2 weeks of age (MFI 7.07 vs. 3.26, p=0.0017). Elevated levels of regulatory T cells following IUHCT also had a functional effect in the GVHD model (Figure 2). Mice that had undergone IUHCT (group 1) demonstrated a trend toward improved survival compared to naive mice when injected with B6 BM at P0. Naive mice injected at P0 with B6 BM plus CD4+ splenocytes from chimeric mice (group 2) demonstrated significant improvement in survival compared to naive recipients of B6 BM alone (p=0.049). Although we detected no increase in traditional Tregs after IUHCT alone, we noted a 3-fold increase in traditional Tregs of host origin in chimeric animals at 48 hours post-DLI (25.5% vs. 8.3%, p<0.001).
Conclusion: The induction of tolerance following IUHCT is important for maintaining successful long-term engraftment and preventing GVHD. We demonstrate an increase in nontraditional regulatory T cells following IUHCT which can minimize GVHD as well as an increase in traditional Tregs following DLI in an established model of complete allogeneic engraftment. These studies suggest an important role for regulatory T cell populations in the induction of tolerance following IUHCT. They are significant in light of a potential obstacle to the clinical translation of IUHCT: the window of central tolerance induction in humans occurs at a gestational age that will pose significant technical challenges. Augmentation of regulatory T cell-dependent peripheral tolerance is one approach by which IUHCT could be delayed to a technically feasible point later in gestation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal