Abstract
Background: There is a well-known risk of developing multiple myeloma in plasmacytoma, especially in solitary bone tumors. However, the risk of other cancers is not clear. The aim of this study was to estimate the risk of second cancers in patients with plasmacytoma, as compared to general population, and patients with multiple myeloma.
Methods: Surveillance, Epidemiology and End results (SEER) 18 dataset was queried to identify patients (age
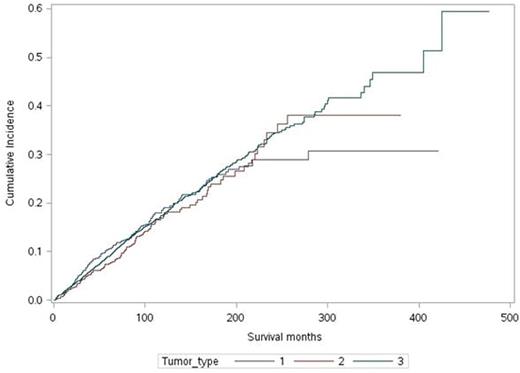
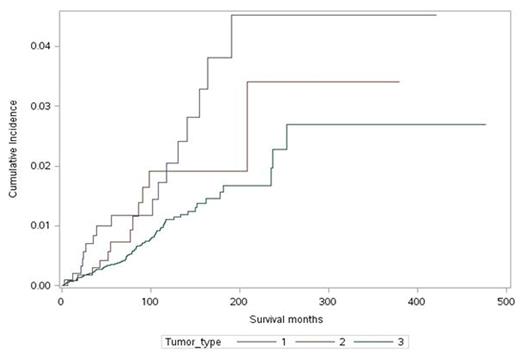
Results: With a follow-up of 13,392 person-years, 331-second cancers were diagnosed in 2046 plasmacytoma survivors (1155 SPB and 891 extraosseous plasmacytoma). The risk of subsequent solid tumors was not higher compared to age and sex matched background population with a SIR of 1.02 (95 % CI .88-1.17 AER 2.23/10,000). The risk was higher for developing multiple myeloma (SIR 30.8 25-38 AER 67/10,000), leukemia (SIR 3.4, 95% CI; 2-5.2 AER 10/10,000) and non-Hodgkin's lymphoma (NHL) (SIR 3.2, 95 % CI 2.1-4.7 AER 13.4/10,000) in "two-month" survivors of plasmacytoma as compared to general population. The risk of developing solid tumors was similar in SPB (SIR 1.07, 95% CI; .87-1.30 AER 9/10,000) and extraosseous (SIR .98, 95% CI; .77-1.19 AER -5/10,000) plasmacytoma. However the risk of transformation to multiple myeloma was 3.7 fold (hazard ratio 3.7, 95% CI; 2.2-6.3) (p<.001) higher in survivors of SPB (SIR 47.3 95% CI; 37-59 AER 103/10,000) than extraosseous plasmacytoma (SIR 13.6 95% CI; 8.3-21 AER 29/10,000). The mean duration for progression to multiple myeloma was significantly shorter for SPB; 348 months (95% CI; 340-356) vs 404 months (95% CI; 395-415) (p=<.001). The cumulative incidence of subsequent malignancies in the study cohort at 15 years was 24.5% (95% CI; 20.1-29.8) for SPB and 25.9 % (95% CI; 21.8-30.2) for extraosseous plasmacytoma. The risk of second malignancies in survivors of plasmacytoma was similar to survivors of multiple myeloma, and the cumulative incidence of second cancers did not differ according to the type of tumor (extraosseous, SPB, or multiple myeloma) (P=0.48). On a subgroup analysis risk did not change after excluding plasmacytoma survivors who developed multiple myeloma. The risk of NHL was significantly higher for patients with extraosseous plasmacytoma, with 42.3% (24.5-75.6%) of these patients developing NHL after 15 years. This stands in contrast to the 16.2% (11.6-20.1) of multiple myeloma survivors who subsequently developed NHL. The patients with SPB were at intermediate risk.
Conclusion: The risk of second cancers in plasmacytoma survivors is not significantly different from the risks for second cancers in survivors of multiple myeloma. The extraosseous plasmacytoma survivors are at higher risk of developing NHL, which suggests further study. The risk of transformation into multiple myeloma, despite lower than solitary plasmacytoma of bone, is still very high (13.6 times than general population), and thus active surveillance by treating physicians is mandatory.
Cumulative incidence of second cancers in survivors of 1.Extraosseous plasmacytoma
2. Solitary plasmacytoma of bone (SPB) 3. Multiple myeloma.
Cumulative incidence of second cancers in survivors of 1.Extraosseous plasmacytoma
2. Solitary plasmacytoma of bone (SPB) 3. Multiple myeloma.
Cumulative incidence of non-Hodgkin's lymphoma in survivors of 1.Extraosseous plasmacytoma
2. Solitary plasmacytoma of bone (SPB) 3. Multiple myeloma.
Cumulative incidence of non-Hodgkin's lymphoma in survivors of 1.Extraosseous plasmacytoma
2. Solitary plasmacytoma of bone (SPB) 3. Multiple myeloma.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal