Abstract
Introduction
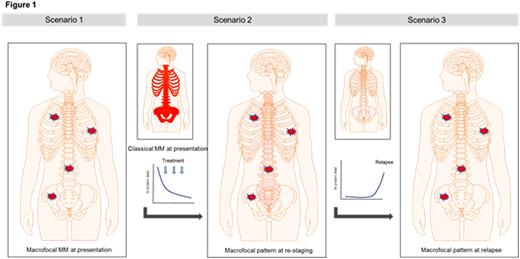
Functional imaging of Multiple Myeloma (MM) is redefining our knowledge of disease patterns. A pattern, termed macrofocal MM (macro MM), is defined by the presence of focal lesions and the absence of significant intervening bone marrow (BM) infiltration. At presentation, macro MM constitutes a distinct disease entity likely being associated with a favorable prognosis, although current evidence to support this is limited. Following first-line therapy, macrofocal patterns of disease emerge also in patients that initially presented with classical MM. In these patients the systemic BM involvement disappears in follow up examinations during treatment whereas focal lesions persist. In a third scenario, macrofocal patterns occur at overt relapse representing a patchy type of MM progression (Figure 1). The prognostic impact of a macrofocal pattern at these various disease stages is largely unknown. Therefore, we analyzed the clinical outcome and biological features of macro MM at different treatment stages.
Patients and Methods
279 patients met the criteria of macro MM. Of those, 56 were at initial presentation, 48 at restaging following first line therapy, and 175 at relapse. Generally, macrofocal lesions were present in both positron emission tomography and magnetic resonance imaging. All first-line patients were treated with multi-agent induction therapy, autologous stem cell transplantation and received maintenance within prospective trials. Outcome results were compared to a set of cases with classical MM matched for age, gene-expression based (GEP) risk group, and treatment protocol.
Results
Macro MM at presentation is rare, constituting 6% of patients in the time period examined. The vast majority showed GEP-based low risk (94%). Age, Ig-type, and sex were not significantly different between macro MM and classical MM. With a median follow up of 8.6 years, only 10 of the macro MM patients relapsed. Compared to a matched-pair MM group, progression-free survival (PFS) and overall survival (OS) were significantly better in the macro MM group (P= 0.01 and 0.04 for PFS and OS, respectively). Thus macro MM at presentation constitutes a low risk form of MM.
Focusing on the 10 macro MM cases who relapsed, no specific risk profile could be identified except >26 focal lesions on MRI was associated with a shorter PFS (P=0.04) but not with OS. Of note, although focal lesions frequently responded slowly, the time to response was not associated with outcome.
To elucidate whether there are biological differences between MM cells in focal lesions and at differentially involved BM sites, we analyzed a set of 16 patients with paired samples from macrofocal lesions and iliac crest BM aspirates. No difference in a GEP based proliferation index was seen between the two sites. After correction for multiple testing we did not observe gene expression differences between them. A candidate gene study including a set of 27, myeloma relevant, adhesion molecules also did not reveal expression differences.
In contrast to the situation at presentation, macrofocal patterns at restaging during initial therapy showed a 70% cumulative 24 months relapse incidence. The outcome of these cases was significantly worse in comparison to matched controls (P=0.02 and 0.02 for PFS and OS, respectively). Of note, all patients with macro MM showed an objective response at the time of imaging with 9 of 46 cases meeting the IMWG criteria for CR.
Performing a similar analysis of patients with macro MM at relapse showed that 25% of patients presented with that pattern; a surprisingly high proportion. Extramedullary involvement was common (41%). Of note, 36% of patients repeatedly showed macrofocal patterns at subsequent relapses. PFS and OS at 2 years from macrofocal relapse were 24% and 39%, respectively. A matched group OS comparison was not possible since number of relapses and treatments were too different among the patients.
Conclusions
Macro MM at presentation seems to be an early stage of MM with an excellent prognosis. In contrast, a macrofocal pattern at restaging is associated with poor prognosis and early relapse. At this disease stage residual focal lesions may represent drug resistant clones. At overt relapse a macrofocal pattern was frequently seen, highlighting the need to integrate advanced imaging tools into the standard work up and indicating an important confounder of standard minimal residual disease diagnostics in MM.
Barlogie:Signal Genetics: Patents & Royalties. Davies:Janssen: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Celgene: Consultancy, Honoraria. Morgan:Celgene: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria; Bristol Meyers: Consultancy, Honoraria; Janssen: Research Funding; Univ of AR for Medical Sciences: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal