Abstract

Background: Venetoclax (VEN) is a potent, highly selective, orally bioavailable small-molecular BCL2 inhibitor that is FDA-approved for patients (pts) with chronic lymphocytic leukemia (CLL) that harbors del(17p) and who have received ≥1 prior therapy. VEN monotherapy induces objective response in ~80% of pts (16-20% complete remission by investigator) with relapsed/refractory (R/R) CLL, including del(17p) CLL (Roberts et al, 2016; Stilgenbauer et al, 2016). Safety of VEN monotherapy was evaluated using an integrated dataset from pts with CLL.
Methods: Pts were included if they received at least one dose of 400 mg VEN as target dose in the M12-175 (first in human), M13-982 (del[17p] CLL), or M14-032 (prior ibrutinib or idelalisib) Phase I or II studies. All started with weekly dose ramp up to 400 mg daily over 4-5 weeks and continued VEN until disease progression/discontinuation.
Results: Overall, 296 pts were included in the analysis: median age was 66 years (range: 29-85), 94% had ECOG score 0-1, 53% had Binet stage A, 27% B, and 19% C. 66% had del(17p) CLL, 77% had unmutated IGHV, and 69% had β-2 microglobulin >3 mg/L. Pts had received a median of 3 prior therapies (range: 0-12) and 94 (32%) had received prior ibrutinib or idelalisib. A history of cytopenias was common, with neutropenia in 52 (18%) pts, anemia in 118 (40%), and thrombocytopenia in 80 (27%). Forty-six (16%) pts were on G-CSF support prior to enrollment.
At the time of analysis, median duration on VEN was 13 months (range: 0-50), with 55% pts receiving VEN daily for >1 year. Common AEs (any grade) were neutropenia (41%), diarrhea (39%), nausea (36%), anemia (29%), fatigue (26%), and upper respiratory tract infection (23%). The most common Grade 3/4 AEs were neutropenia (37%), anemia (15%), and thrombocytopenia (14%). Grade 3/4 infections were reported for 19% of pts. Common serious AEs were pneumonia and febrile neutropenia (5% each); most serious AEs occurred within the first 3 months on VEN. Twenty-five deaths were reported: 13 due to disease progression and 12 were treatment-emergent AEs due to complications related to underlying CLL (most common were infections [4]); none were attributed by the investigator to VEN. The safety profile was similar when analyzed by subgroups, including age, sex, race, or prior ibrutinib/idelalisib.
Four pts had AEs of TLS, though only one met Howard criteria for laboratory TLS (decreased calcium and increased phosphate). No clinical TLS was observed. All events occurred during the 5-week dose ramp up and pts interrupted VEN dosing for median of 3 days (range: 1-5), though all restarted VEN to reach 400 mg. Events were managed by IV hydration and standard of care for laboratory abnormalities.
A major reason for VEN interruptions/reductions was neutropenia, with most dose adjustments occuring within the first 3 months on study. Neutropenia was managed by standard supportive care measures, including G-CSF support for 136 (46%) pts during this time.
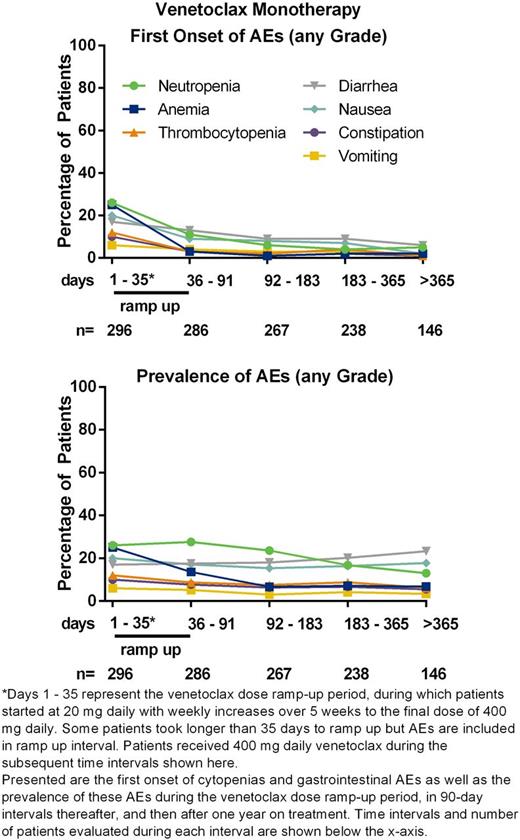
Time of first onset for most hematologic toxicities (any grade) occurred during dose ramp up (Figure). First onset of new AEs within or after 3 months on VEN (shown as within/after 3 months) was 34%/7% for neutropenia, 27%/3% anemia, and 14%/5% thrombocytopenia. This temporal pattern is likely due to improving CLL disease control though for some pts this may be the result of increasing time off prior myelosuppresive chemotherapy. Grade 4 neutropenia was reported in 71 (24%) pts and median time to event was 28 days (range: 2-416); 48/71 (67%) had Binet C at screening and median time to event was 23 days (range: 2-415). Grade 4 neutropenia required dose reductions for 21% of pts, 80% received G-CSF support, and 1 event led to study discontinuation. Grade 4 thrombocytopenia occurred in 32 (11%) pts (23 had Binet C) and Grade 4 anemia in 2 (2%) pts (both Binet C).
Gastrointestinal toxicities were mainly Grade 1/2, with 60% new events reported in the first 3 months vs 11% reported > 3 months (Figure). No late toxicity signal has been observed in pts receiving >1 year of therapy.
Conclusions: The safety profile of 400 mg VEN daily was consistent across pts with CLL pooled from 3 studies and remains acceptable with longer follow up in this larger population. No clinical TLS was observed and one event of laboratory TLS was manageable. The majority of AEs, including cytopenias (most common Grade 3/4 AEs), occurred during the first months of VEN and onset of AEs decreased over time in pts with emergent toxicities.
Seymour:AbbVie Inc.: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Gilead: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Genentech: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees. Davids:Genentech: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria; Gilead: Honoraria; Pharmacyclics: Consultancy, Honoraria, Research Funding; Infinity: Honoraria, Research Funding; TG Therapeutics: Honoraria, Research Funding; Abbvie: Consultancy, Honoraria. Roberts:AbbVie: Research Funding; Genentech: Research Funding; Genentech: Patents & Royalties: Employee of Walter and Eliza Hall Institute of Medical Research which receives milestone payments related to venetoclax; Janssen: Research Funding; Servier: Research Funding. Hallek:GSK: Research Funding; Mundipharma: Research Funding; Janssen: Research Funding; Celgene: Research Funding; Gilead: Research Funding; AbbVie: Consultancy, Honoraria, Research Funding; Roche: Consultancy, Honoraria, Research Funding; Genentech: Consultancy, Honoraria. Wierda:Genentech: Research Funding; Abbvie: Research Funding; Novartis: Research Funding; Acerta: Research Funding; Gilead: Research Funding. Hillmen:Pharmacyclics: Research Funding; Janssen: Honoraria, Research Funding; Roche: Honoraria, Research Funding; Gilead: Honoraria, Research Funding; Abbvie: Research Funding. Gerecitano:Samus: Consultancy, Honoraria; Bayer: Consultancy, Honoraria; Genentech: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria. Cerri:AbbVie: Employment. Potluri:AbbVie: Employment. Kim:AbbVie: Employment. Busman:AbbVie: Employment. Verdugo:AbbVie: Employment, Other: may own stock. Humerickhouse:AbbVie: Employment. Best:AbbVie: Employment. Desai:AbbVie: Employment. Stilgenbauer:Sanofi: Consultancy, Honoraria, Other: Travel grants , Research Funding; AbbVie: Consultancy, Honoraria, Other: Travel grants, Research Funding; Boehringer Ingelheim: Consultancy, Honoraria, Other: Travel grants , Research Funding; Novartis: Consultancy, Honoraria, Other: Travel grants , Research Funding; Hoffmann-La Roche: Consultancy, Honoraria, Other: Travel grants , Research Funding; Genentech: Consultancy, Honoraria, Other: Travel grants , Research Funding; Amgen: Consultancy, Honoraria, Other: Travel grants, Research Funding; Celgene: Consultancy, Honoraria, Other: Travel grants , Research Funding; GSK: Consultancy, Honoraria, Other: Travel grants , Research Funding; Genzyme: Consultancy, Honoraria, Other: Travel grants , Research Funding; Mundipharma: Consultancy, Honoraria, Other: Travel grants , Research Funding; Pharmacyclics: Consultancy, Honoraria, Other: Travel grants , Research Funding; Janssen: Consultancy, Honoraria, Other: Travel grants , Research Funding; Gilead: Consultancy, Honoraria, Other: Travel grants , Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal