Abstract

Background
Loss of chromosome Y (-Y) is observed in 4-10% of male MDS patients as a single cytogenetic abnormality, and is associated to a better outcome. -Y is also known to be an age related phenomenon occurring in 8-10% of elderly men. The clinical significance of -Y in MDS has been a matter of discussion. However, there is increasing evidence that -Y involves the clonal population in MDS cases, and is more likely to be associated with a hematological malignancy when it involves a greater number of metaphases.
Aims
In this study we aimed to 1) analyze the prognostic impact of -Y in the context of the IPSS-R cytogenetic classification, 2) evaluate the clinical significance of the percentage of metaphases with isolated -Y, 3) test whether finding -Y may predispose to over diagnose MDS in patients with borderline morphological features.
Methods
We evaluated 3581 male patients from the Spanish Registry of MDS with a diagnosis of MDS or CMML (WHO 2001). Patients with isolated -Y and normal karyotype by conventional cytogenetic analysis were selected. The main study outcomes were survival from diagnosis and transformation into acute myeloid leukemia (AML). Survival curves were drawn using the Kaplan-Meyer method and compared by log-rank test. The cumulative incidence of AML was estimated by taking non AML-related death as a competing risk. Statistical comparisons were done by the Mann-Whitney U-test for continuous data, and the chi-square test for categorical factors. Stata, version 11, software (www.stata.org) was used for the statistical analysis.
Results
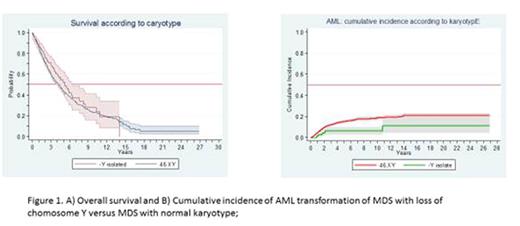
Isolated -Y was identified in 177 patients (-Y group) and compared with the 2246 male patients with normal karyotype (46,XY group). The median age for the whole series was 74 years old (IQR 67-80). -Y patients were found to be older than patients in the 46,XY group with a median (IQR) of 78 (74-83) versus 74 (66-79) years old, respectively (n=0.0001). There was no difference between both groups in terms of hemoglobin concentration, neutrophil and platelet counts at diagnosis. Percentage of bone marrow (BM) blasts was significantly lower in the -Y group (median (IQR): 2(0-3) vs. 2(1-5), respectively; p=0.003). Differences in distribution by WHO 2001 classification of MDS were not found between the two groups. After a follow-up of 2,190 patient-years, 1684 (69.5%) patients had died and the median actuarial survival was 3.6 years (95% C.I, 3.3-3.9). A trend towards a larger median survival in the -Y group versus 46,XY group was observed, since it not reached statistical significance (5.2 years [95% CI, 3.89 to 6.40] versus 4.26 years [95% CI, 3.89 to 4.59], respectively) (P=0. 17; Fig. 1A). After a median follow-up of 1.6 years (IQR: 0.8 - 3.7) from MDS diagnosis, 296 patients had progressed to AML, 901 had died without AML, and 1224 were censored alive without transformation. -Y was associated with a decreased incidence of AML at univariate analysis (figure 1B), and after adjustment for the percentage of BM blasts (SHR: 0.46; 95%CI: 0.24-0.88; p=0.02). Within the -Y group, neither survival nor the risk of leukemic transformation were influenced by the percentage of aberrant metaphases (>75% vs, ≤ 75%). From the whole series, only 6.4% of the cases were classified as not having a "MDS strong phenotype", defined by the presence of megakaryocytic dysplasia, more than 5% blasts in the bone marrow, or more than 15% ring sideroblasts. These cases were uniformly distributed between the two groups, suggesting that the better outcome in the -Y group cannot be explained by enrichment in cases misdiagnosed as MDS.
Conclusions
Our results derived from the largest series of patients with loss of chromosome Y support the current recommendation of classifying patients with -Y within the very good risk category of the IPSS-R for MDS and rule out a selection bias as a possible explanation of this better outcome. An analysis of the molecular basis of MDS with isolated -Y would be of interest as it may provide a biological basis of protection against AML progression.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal