Introduction: CD20-negative subtypes of diffuse large B-cell lymphoma (DLBCL) are rare, aggressive malignancies. Recently, cancer registries in the United States (US) have distinguished specific subtypes of CD20-negative DLBCL: since 2004-primary effusion lymphoma (PEL), and since 2010-plasmablastic lymphoma (PBL), ALK+ large B-cell lymphoma (ALK+LBCL), and large B-cell lymphoma arising in HHV8+ multicentric Castleman disease (HHV8+MCD). Our objective was to provide the first large-scale analysis of those lymphomas, focusing on their epidemiology, treatment, and outcomes relative to unspecified DLBCL (DLBCL-NOS).
Methods: Using data from the National Cancer Data Base (NCDB), we selected patients with PEL (2004-2013) and with PBL, ALK+LBCL and HHV8+MCD (2010-2013), and compared their characteristics and management with contemporaneous DLBCL-NOS. We analyzed receipt of chemotherapy in subsets defined by histology and HIV status. We then compared overall survival (OS) from diagnosis in a multivariate Cox model stratified by age, sex, race, stage, and HIV status, reporting adjusted hazard ratios (HR) with 95% confidence intervals (CI). Predicted survival of DLBCL-NOS matched by the same variables was calculated from flexible parametric models.
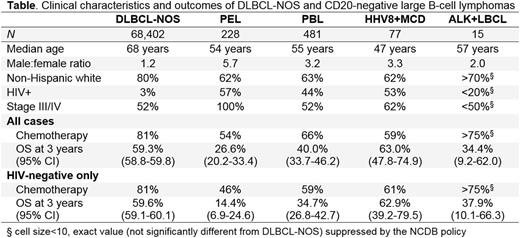
Results: Of the 801 identified cases, 228 were PEL, 481 PBL, 77 HHV8+MCD, and 15 ALK+LBCL. We compared them with 68,402 contemporary cases of DLBCL-NOS. Patients with CD20-negative lymphomas were significantly younger on average (Table), more often male, HIV+ (except for ALK+LBCL), and less frequently non-Hispanic whites (NHW). Among patients with PEL, PBL, and HHV8+MCD, those who were HIV+ were significantly younger than HIV-negative (median age, 45 versus 70 years), more often male (88% versus 70%), less often NHW (49% versus 80%), and had more B symptoms (44% versus 21%, all P<.0001), but stage distribution did not significantly differ according to HIV+ status (P=.09). PEL cases with specified primary site were pleural/thoracic in 82%, and peritoneal/abdominal in 18%. Among PBL cases, 21% arose from the head/neck area, 21% from gastrointestinal tract, and 58% from other (or unspecified) areas. Almost all ALK+ cases, and 79% of HHV8+MCD, were nodal, whereas 53% of PBL cases were extranodal.
Compared with DLBCL-NOS, the use of chemotherapy was significantly less frequent among patients with PEL, PBL, HHV8+MCD (Table, all P<.0001), but not among those with ALK+LBCL (P=.96). In contrast to DLBCL-NOS, HIV+ status was associated with a higher likelihood of receiving chemotherapy in PEL (60%, versus 46% for HIV-negative, P=.035) and PBL (75% versus 59%, respectively, P=.0003), without a significant difference in HHV8+MCD (59% versus 61%, respectively, P=.82).
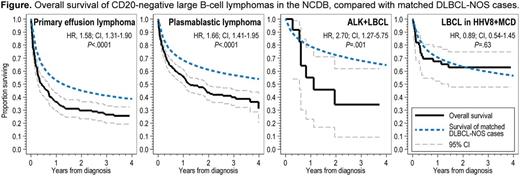
Compared with matched DLBCL-NOS cases, OS was significantly worse for patients with PEL, PBL or ALK+LBCL, but not for those with HHV8+MCD (Table, Figure). HIV+ status was not associated with worse OS in PEL (P=.22), PBL (P=.39) or HHV8+MCD (P=.56) after adjusting for age difference. Advanced stage was associated with worse OS in PBL (P=.0002), but not in ALK+LBCL (P=.98) or HHV8+MCD (P=.27).
Conclusions: This large analysis of CD20-negative DLBCL subtypes using nationwide registry data reveals new information about these rare disorders. While PEL, PBL and HHV8+MCD are strongly associated with HIV infection, ALK+LBCL is not, although it still occurs in younger patients with male predominance. HIV+ patients with PEL, PBL, or HHV8+MCD do not have worse survival outcomes than those who are HIV-negative. Furthermore, despite the association with HIV, survival of HHV8+MCD is overall not worse than that of matched DLBCL-NOS cases. In contrast, the other subtypes have a significantly worse survival compared with DLBCL-NOS, highlighting the unmet need for improved therapeutic approaches. ALK+LBCL is either exceptionally rare, or underdiagnosed in the current practice, and has poor OS, warranting studies of ALK-targeted therapy.
Castillo:Otsuka: Consultancy; Abbvie: Research Funding; Pharmacyclics: Honoraria; Millennium: Research Funding; Janssen: Honoraria; Biogen: Consultancy. Olszewski:TG Therapeutics: Research Funding; Genentech: Research Funding; Bristol-Myers Squibb: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal