Abstract
In the updated 2016 revision of WHO classification, pure erythroid leukemia (PEL) is still viewed as a sole entity without any change of definition. However, erythroleukemia (erythroid/myeloid type) (previously defined as myeloid neoplasms with erythroid predominance [EP] and myeloblasts ≥ 20% or < 20% but ≥ 20% of nonerythroid cells) has been removed. The former is now recognized as acute myeloid leukemia, not otherwise specified (AML-NOS), and the latter as no longer acute erythroid leukemia (AEL) but MDS.
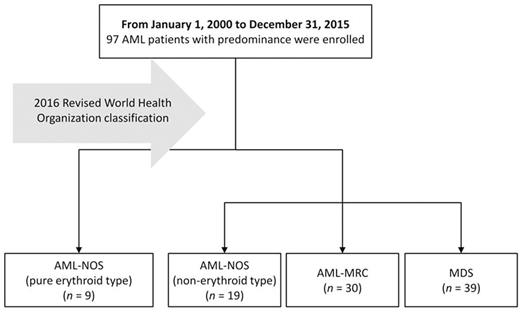
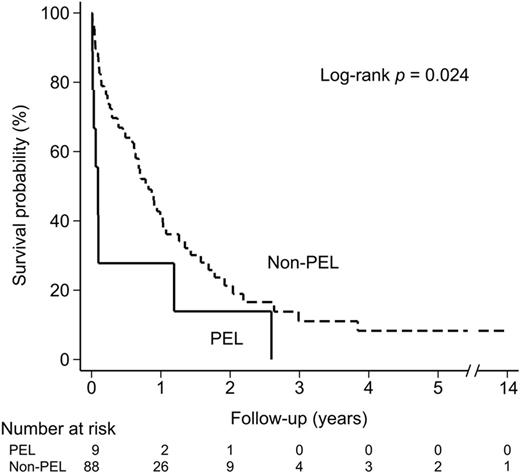
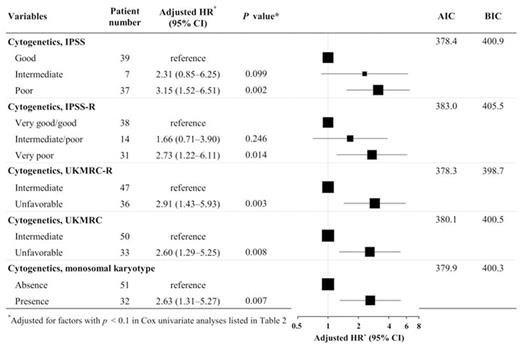
Such a change in the updated classification provides us the rationale to conduct this cohort study of patients with AML with EP (AML-EP). We report the impact on survival outcomes and the risk factors for mortality in these patients based on the 2016 WHO classification. A total cohort of 97 consecutive cases of acute myeloid leukemia with erythroid predominance (AML-EP) between 2000 and 2015 was enrolled. Following 2016 WHO classification, AML-EP patients were classified into four groups (Figure 1). Nine PEL patients had more dismal outcomes (median OS: 1 month) as compared with non-PEL patients (Figure 2) and showed more bone marrow fibrosis, worse performance status (PS) and higher serum lactate dehydrogenase (LDH) at diagnosis. In the univariate analysis, risks of death were PEL diagnosis, worse cytogenetic risks, bone marrow fibrosis, leukocytosis, anemia, hypoalbuminemia, high (LDH), and poor PS. In the multivariate analysis, independent predictors of death were PEL diagnosis (adjusted hazards ratio [AHR] 3.00, 95% confidence interval [CI] 1.02¡V8.88, p = 0.029), very poor cytogenetic risk by IPSS-R (AHR 2.73, 95% CI 1.22¡V6.11, p = 0.014), hypoalbuminemia (< 3.7 g/dl) (AHR 2.30, 95% CI 1.09¡V4.83, p = 0.028) and high serum LDH (≥ 250 U/L) (AHR 2.31, 95% CI 1.25¡V4.28, p = 0.008). Based on the karyotype, patients were stratified to different cytogenetic risk groups according to the United Kingdom Medical Research Council (UKMRC) criteria for AML, the revised United Medical Research Council (UKMRC-R) criteria for AML, the International Prognostic Scoring System (IPSS) for MDS, the revised International Prognostic Scoring System (IPSS-R) and the presence or absence of monosomal karyotypes. Cytogenetic risks groups determined by UKMRC-R showed the best ability to predict survival outcomes of AML-EP patients (Figure 3). The outcome of PEL was independently much worse than that of non-PEL. Allogeneic HSCT was administered to 10 patients (one PEL, one AML-MRC, three AML-NOS and five MDS cases), whose disease statuses at transplantation were refractory disease for one and complete remission for nine. As compared to supportive care, the mortality among AML-EP patients did not differ from that of the patients receiving allogenic hematopoietic stem cell transplantation, curative chemotherapy or non-curative chemotherapy.
In conclusion, after the 2016 WHO classification was published, only PEL were kept as belonging to neoplasms originated from neoplastic erythroid lineage. This retrospective cohort study reports the clinical features, biological data and survival outcomes of patients with AML-EP and identified PEL diagnosis, very poor cytogenetic risk group of IPSS-R, high serum LDH and low serum albumin as independent predictors for death. Cytogenetic risks groups determined by UKMRC-R showed the best ability to predict survival outcomes of AML-EP patients. The outcome of PEL was independently much worse than that of non-PEL.
Survival curves of patients of pure erythroid leukemia and others
PEL, pure erythroid leukemia
Survival curves of patients of pure erythroid leukemia and others
PEL, pure erythroid leukemia
Impact of the cytogenetic risk group on mortality
HR, hazards ratio; CI, confidence interval; AIC, Akaike information criterion; BIC, Bayesian information criterion (the lowest level represents the best prediction ability)
*Adjusted for factors with a p < 0.1 in the Cox univariate analysis.
Impact of the cytogenetic risk group on mortality
HR, hazards ratio; CI, confidence interval; AIC, Akaike information criterion; BIC, Bayesian information criterion (the lowest level represents the best prediction ability)
*Adjusted for factors with a p < 0.1 in the Cox univariate analysis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal