Abstract
Introduction:
The median age of diagnosis for Acute Myeloid Leukemia (AML) is just under 70 years. The most common initial management strategies are induction with intensive chemotherapy (IC), low-dose chemotherapy (LD), hypomethylating agents (HMA), or best supportive care (BSC). Since many studies include a mixture of patients, the outcomes of patients aged over 70 following induction are not well known, and clinicians vary widely in their estimation of risk and benefits of treatment for these patients. The aim of this systematic review and meta-analysis was to identify all randomized controlled trials (RCT) and non-randomized studies (NRS) which had data available for patients aged over 70 and to report outcomes based on induction type.
Methods:
A comprehensive search of MEDLINE and Cochrane databases was performed from inception until June 30, 2015. Two authors independently reviewed all references and included studies which enrolled newly diagnosed patients aged over 70. To minimize anecdotal evidence, only RCT enrolling more than 20 older patients per arm and NRS enrolling more than 50 older patients were included. Data were extracted independently using a standardized data collection form. Every effort was made to contact original investigators to obtain data not available in publications. Outcome data were collected by induction treatment type and a proportional meta-analysis was performed. All results are reported as a pooled proportion and 95% confidence interval (CI). Heterogeneity between studies was measured using I2 with >50% indicating high heterogeneity.
Results:
Our search yielded 11,259 references of which 61 RCT and 60 NRS met inclusion criteria. Following correspondence with the investigators for additional information, 33 RCT (5233 patients) and 26 NRS (6494 patients)(total: 59 studies with 11,727 patients) were included.
In RCTs, age ranged from 70 to 94 and in NRS from 70 to 95. Performance status was reported by 17 RCT and 14 NRS. Cytogenetics was reported in 14 RCT and 14 NRS. Comorbidities were reported by 1 RCT and 3 NRS, each of which reported all 3 covariates.
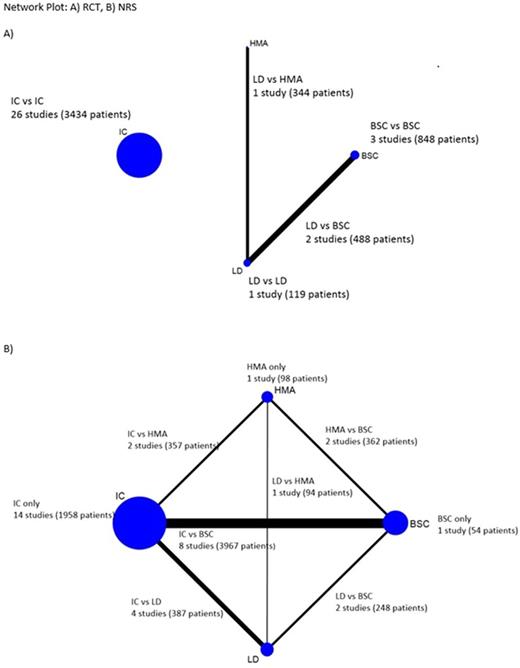
The comparison networks are shown in the figure. The majority or RCT (26/33; 79%) compared two IC treatments. Two RCT compared LD to BSC and one RCT compared HMA to LD. Similarly, the majority of NRS (14/26; 54%) studied only IC. Eight NRS compared IC to BSC, two NRS compared IC to HMA, and four NRS compared IC to LD.
Although 26/33 RCT and 20/26 NRS reported some survival data, the reporting period differed widely. One-year survival could be extracted from 8 RCT and 7 NRS. For IC, the 1-year survival tended to be lower in NRS: 45% (95% CI 29-62%, I2 93%) vs 28% (20-36%, I2 68%). For LD: 11% (6-18)in one RCT. For HMA: 45% (35-55) in one NRS. For BSC: 16% (14-19) in 2 RCT and 11% (4-37) in 1 NRS.
Complete response rates were reported in 30/33 RCTs and 23/26 NRS. For IC, it was 44% (39-49) in RCTs and 42% (38-47) in NRS. For LD, 18%(13-25) and 21%(0-50). For HMA, 17%(12-22) in 2 NRS. For BSC 13%(12-19) and 1%(0-3). Heterogeneity was significant throughout.
Early death (at 30 days) was reported in 19 RCT and 17 NRS. For all regimens, the percentage is 15-20%, with significant heterogeneity. The one NRS with HMA had 1% early deaths.
Results stratified for cytogenetics, performance status, and comorbidity will be presented.
Conclusions:
Our systematic review provided the largest clinical cohort of AML patients aged 70+ to date. Although prognostic factors and outcomes are heterogeneously reported, differences in outcomes amongst treatment types emerged. This large dataset, while not lending itself to homogeneous results from meta-analysis, provides a basis for a decision analysis model with formal sensitivity testing, in order to help clinical decision making in AML patients 70 and older. We also identified a need for more studies comparing IC with other treatment modalities, notably HMA, and the need for a more systematic inclusion of covariates such as cytogenetics/molecular data, functional status, and comorbidity.
This research is supported by NIH grant 1-R01-CA168677-01A1
Extermann:GTx: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal