Abstract

Background:
There is demonstrated benefit when administering fluoroquinolones as infection prophylaxis in neutropenic patients; however, side effects, drug interactions and increasing drug resistance necessitate investigation toward safe and effective alternative therapies. This study investigates the use of oral third generation cephalosporins as antibacterial prophylaxis during chemotherapy-induced neutropenia to establish knowledge on alternative treatment options.
Methods:
A retrospective chart review was performed to compare incidence of febrile neutropenia and documented infection rates in Acute Myeloid Leukemia (AML) and intermediate to high International prognostic scoring system (IPSS) risk myelodysplastic syndrome (MDS) patients receiving antibacterial chemoprophylaxis at Mayo Clinic between January 2006 and April 2016. Patients were included if they were 18 years or older, had a diagnosis confirmed on bone marrow biopsy, received induction or first relapse induction-remission chemotherapy regimens and then subsequently were prescribed fluoroquinolone or an oral third generation cephalosporin prophylaxis for anticipated profound and prolonged neutropenia. The main regimens prescribed were cytarabine + anthracycline (7+3), daunorubicin + cytarabine + nilotinib, mitoxantrone + etoposide + cytarabine, all-trans-retinoic acid (ATRA) + anthracycline, all-trans-retinoic acid (ATRA) + arsenic, clofarabine + cytarabine, or an investigational trial. After meeting inclusion criteria the treatment arms were matched via Charlson comorbidity index ( ± 3) and age ( ± 5). Patients with a documented infection 48 hours after switching from either broad spectrum antibiotics to antibacterial prophylaxis, or from levofloxacin prophylaxis to an oral third generation cephalosporin were excluded from the study. All patients provided consent for review of their medical records for research purposes. This study was approved by the Mayo Foundations institutional review board.
Results:
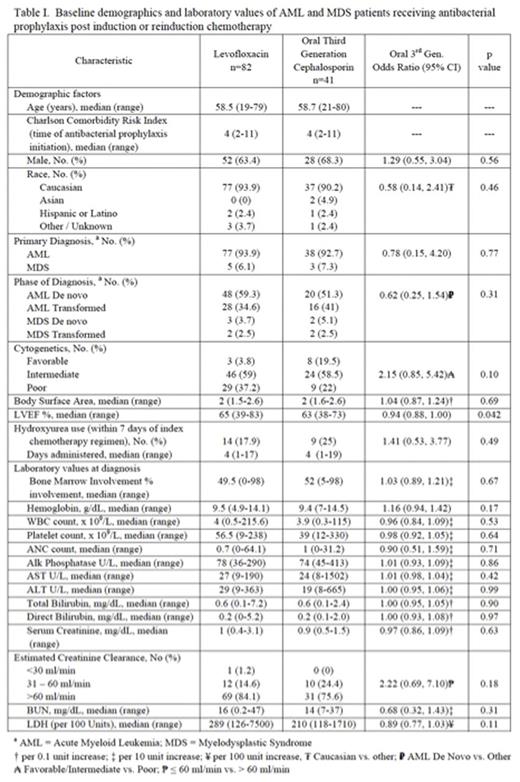
A total of 565 patients admitted to Mayo Clinic inpatient leukemia service for chemotherapy and concurrently prescribed antibacterial prophylaxis with either levofloxacin or an oral third generation cephalosporin were screened between January 1, 2006 and April 1, 2016. Of those screened 397 patients met the inclusion criteria, and subsequently 123 patients were matched via Charlson comorbidity index and age. Patient characteristics are presented in Table I. Of the 123 study patients, 80 (65%) were male, and the median age was 58.6 years (IQR: 53.3-68.5). The population was comprised of 115 (93.5%) patients with AML, and 8 (6.5%) patients with MDS.
By 30 days after prophylaxis start 109 of the 123 patients developed febrile neutropenia (89.9%, 95% CI: (82.8-94.1)). There was no difference in the risk of febrile neutropenia between those on levofloxacin and those on an oral third generation cephalosporin (hazard ratio [HR] = 1.057, 95% CI: 0.64-1.75, p=0.83). The mean ANC value at the time of febrile neutropenia was 0.47 (SD: 1.4). Documented reasons that patients did not receive an oral fluoroquinolone were QTc prolongation (34.2%), rash (21.1%), tendonitis (2.6%), anaphylaxis (5.3%), drug interaction with a treatment study drug (23.7%), or other (13.1%). Three patients died 30 days or less after the last dose of chemoprophylaxis (40 day survival: 96.6%, 95% CI: 92.7-100); two of the reported deaths were due to infection.
Of the 111 patients who had a documented febrile episode, 40 (36%) had a culture positive infection. Gram positive organisms caused 27 (71.1%) of the infections, 11 (28.9%) were gram negative organisms, and 1 (2.6%) infection was due to an anaerobic organism. There were 3 (7.5%) polymicrobial infections, and 36 (90%) monomicrobial infections. The majority of the patients had bloodstream as the documented site of infection. Of the documented culture positive infections 15 (39.5%) showed resistance to levofloxacin and 6 (15.8%) had resistance to third generation cephalosporins when susceptibility testing was reported.
Conclusions:
These findings demonstrate comparable safety and efficacy of oral third generation cephalosporins compared to fluoroquinolones and contribute to the growing body of literature surrounding antibacterial prophylaxis during chemotherapy-induced neutropenia. Further prospective, randomized investigation is warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal