Abstract
Introduction
Little data exist on the clinical presentation, management and treatment of aplastic anemia (AA) in pregnancy.The aim of this study is to describe the clinical presentation, management and outcomes of patients with AA in pregnancy based on a single centre, North American experience.
Methods
Patients with AA during pregnancy managed at Mount Sinai Hospital, a tertiary care centre in Toronto, Canada, were retrospectively identified through the Special Pregnancy Program database from 1990 to 2014, inclusive. Charts and electronic medical records were reviewed to extract demographics, clinical features, bone marrow biopsy results, paroxysmal nocturnalhemoglobinuria(PNH) status, comorbidities, treatment and transfusion requirements, as well as obstetrical and post-partum outcomes.The Research Ethics Board at Mount Sinai Hospital approved the study.
Results
Between 1990 and 2014, 24 pregnancies were identified in 12 women with AA. Among these, 3 women (5 pregnancies) were excluded from subsequent analysis due to incomplete records. Among the 19 pregnancies in 9 women with AA, 6 women had at least one subsequent pregnancy during the study period.
The initial diagnosis of AA occurred during pregnancy in 5 of the 19 pregnancies in 9 women (Table 1). Four of the 5 women were diagnosed with AA in the first trimester. The presenting signs and symptoms included fatigue (1), chest pain due to severeanemia(1),petechiae(1), hematemesis (1) and in 1 patient the diagnosis was made following a CBC performed for routine prenatal care. Among the 14 pregnancies with a prior diagnosis of AA, 4 were in complete remission (CR) and 6 were in partial remission (PR). In addition, there were 5 pregnancies in 3 women following allogeneic bone marrow transplant (alloBMT). Of these, 3 pregnancies occurred post-alloBMTin CR, 1 in PR and 1 was not in remission. PNH clones were present in 4 of the pregnancies (3 women).
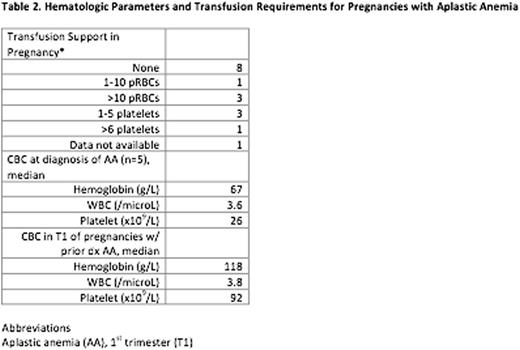
Among the 5 pregnancies with newly diagnosed AA, 3 were treated with cyclosporine during pregnancy and 1 was treated with prednisone alone, all without a response. Transfusion support was required in 10 of the 19 pregnancies, including all 5 pregnancies with newly diagnosed AA (Table 2). In the 5 pregnancies with newly diagnosed AA, the median haemoglobin was 67g/L, median WBC was 3.6/microLand median platelet count was 26x109/L at the time of diagnosis. In the 14 pregnancies with a prior diagnosis of AA, the median haemoglobin, WBC and platelet counts in the first trimester were higher (Table 2).
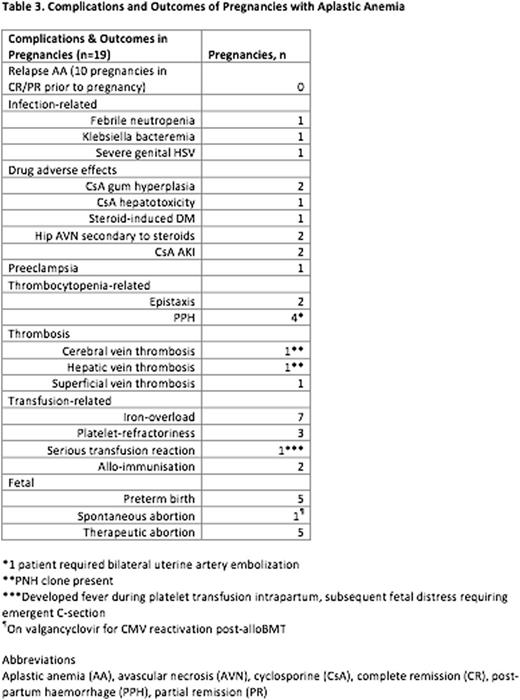
Although there were no maternal deaths, significant complications occurred in 15 of the 19 (79%) pregnancies (Table 3). Four pregnancies (in two women) were not associated with significant complications and these patients were in PR or CR at the onset of pregnancy. Common complications during pregnancy and post-partum included transfusion-related event (13), drug adverse effect (8), bleeding (6), preterm birth (5), thrombosis (3) and infection (3) (Table 3). Most of the pregnancies experienced declining hematologic parameters over the course of pregnancy. However, relapses were not observed among the 10 pregnancies in CR or PR at onset of pregnancy.
There were no spontaneous remissions of AA in the postpartum period. Among the 5 women with newly diagnosed AA in pregnancy, 3 underwentalloBMTand 2 had excellent outcomes with resolution ofcytopeniasand no complications. The third woman who underwentalloBMTsuffered significant complications following transplantation including disseminatedNocardia(brain and lung), renal dysfunction secondary to cyclosporine, acute GVHD of the gastrointestinal tract and liver, pericarditis, iron overload and transfusion dependency.
Conclusions
AA in pregnancy is rare, with 24 pregnancies in 12 women over 24 years in a single, tertiary hospital. AA in pregnancy was not associated with mortality but significant morbidity was seen. In our cohort, no spontaneous remissions of AA were observed post-partum. Further studies with larger sample sizes are required to clarify the natural history of AA in pregnancy and best approach to management to avoid complications during pregnancy and post-partum.
Schuh:Amgen: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal