Abstract
Background:
Androgens have shown encouraging results in the treatment of marrow failure, both in the animal model (Nouv Rev Fr Hematol. 1984, 26;391) and in patients with aplastic anemia (Blood. 1990;76: 2222). A first trial comparing ATG with or without androgens , failed to show improved response and survival in the androgens group (Blood. 1985; 66:184). However, in a second randomized trial , females receiving ATG+androgens had significantly superior response rates (BJH 1993,83:145). High dose ATG (twice the conventional dose) and androgens, was given to 87 patients, with 77% response rate and 78% survival at 5 years (Ann Hematol 2006;85:711). More recently sex hormones have been shown to increase telomerase activity, resulting in elongated telomeres in vitro [ Blood. 2009 114:2236), and in vivo [ N Engl J Med. 2016 19;374].
Aim of the study: The aim of this study was to evaluate the outcome of androgen treatment in patients with Aplastic Anemia (AA) who had received a previous course of ATG and were persistently cytopenic.
Patients and methods: 78 AA patients were selected as having received oral testosterone 40 mg/day 5-7 days/week , because of persistent cytopenia, in 1-3 cell lines. Typically testosterone was added to the ongoing treatment with cyclosporine. Median age was 37 years (9-72) ; there were 28 males and 50 females.. The median Hb level at start of testosterone, was 8.8 gr/dl( 3-14), the median neutrophil counts 1.7 x10^9/L (0.0-8) and the median platelet count 27x10^9/L (1-128). The median interval between ATG treatment and testosterone was 5 months (0-148); the median duration of androgen treatment was 517 days (range 122- 8984) . Patients were classified as non responders ( no hematologic improvement and/or transfusion dependent), partial responders (transfusion independent and improved peripheral blood counts), or complete responders (normalized peripheral blood counts).
Result: Androgen treatment , at this relatively low dose, was well tolerated, with no abnormalities in liver function tests, and no apparent virilization. One patient discontinued testosterone because of intolerance (1,28%). Of the 78 patients treated, 33% (n=23) were classified as non responders, 29% (n=20) as partial responders and 38% (n=26) as completer responders.
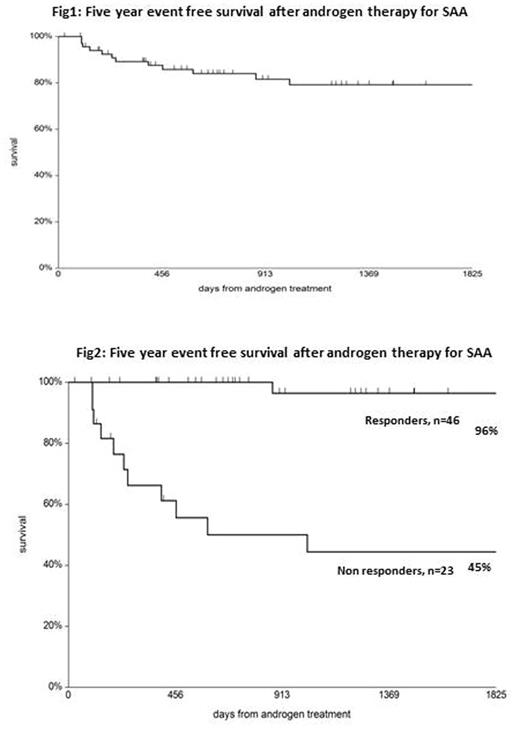
The median hemoglobin level at 90, 180 and 365 days after androgen therapy were respectively: 9.1; 10.6 and 11.4 g/dl; the median neutrophil counts were respectively 2.0; 2.0 and 3.0 x10^9/L; the median platelets were respectively 38, 54, 75 x10^9/L. There was therefore a gradual improvement of peripheral blood counts with time.With a median follow up of 871 days (range 27-8392), the actuarial 5 year survival, free from transplantation or a second course of immunosuppressive therapy, is 85% (Fig.1); it is 96% for responders and 45% for non responders (Fig2); fifteen out 23 non responders were allografted.
Conclusion: The addition of androgen to cyclosporine , improved peripheral blood counts in 67% of our patients, who had failed, or partially failed first line therapy with ATG, with low or absent detectable toxicity. Our results confirm a role for androgens in patients with marrow failure, and this may be relevant for patients eligible for an unrelated transplant, or for older patients discussing an HLA identical sibling transplant. A 3 months course of androgens is still less hazardous as compared to an unrelated donor graft, and may offer the patient an opportunity to achieve transfusion independence without a graft.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal