Abstract

Introduction
Catheter related thrombosis (CRT) is a common complication of central venous catheters (CVCs) in patients with hematological and solid organ cancers. However, little is known about the incidence of CRT in acute leukemia patients and the optimal approach to anticoagulant therapy especially in the presence of concurrent and often prolonged thrombocytopenia. Some of these patients might receive sub-therapeutic anticoagulation with a potentially higher risk of recurrent CRT, device failure and thromboembolic events.
Method
We conducted a retrospective chart review of adult patients with newly diagnosed acute leukemia at Vancouver General Hospital (VGH), Canada from January 2014 to December 2014. The study aimed to determine the incidence of CRT and review the current practice of CRT management. The outcomes were symptomatic thrombotic and bleeding events, catheter complications (e.g. infection), and blood product use. Only objectively confirmed CRT cases were included. The follow up period was from CRT diagnosis to last known date of follow-up.
Results
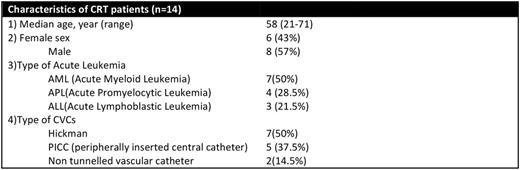
A total of 151 patients were identified, of whom 116 received CVC insertion. Eleven patients (78.5%) received more than one CVC (median 2, range 1-4). Fourteen patients (12%) were diagnosed with symptomatic CRT (table). All CRT events occurred within 30 days (range 4-30 days) after CVC insertion and 85.7% within the first 6 months (range 0.26-6 months) after their diagnosis of acute leukemia. Median follow up of these 14 patients was 447 patient-days (range 13-759). Two patients were lost to follow-up at 13 and 23 days due to transfer of care to other hospitals. Three out of 14 patients died during follow up (at 72, 86 and 372 days, respectively) due to leukemia.
Eleven patients (78.5%) were treated with therapeutic anticoagulation using low molecular weight heparin (LMWH). Three untreated patients had CRT confined to basilic vein. Nine out of 11 patients required LMWH dose reduction due to thrombocytopenia according to our local protocol (1). Full dose weight-based LMWH was administered if platelet count could be maintained above 50 × 109/L (with or without platelet transfusion in acute phase, i.e. within 1 month of CRT diagnosis). For platelet counts between 20 and 50 × 109/L, half-dose LMWH was administered with close monitoring. LMWH was withheld if platelet count was lower than 20 x 109/L in subacute phase, i.e. after 1 month. No patient had recurrent CRT or pulmonary embolism during anticoagulation and follow up.
Bleeding events occurred in 3 (27%) patients during anticoagulation. There was one major bleeding (spontaneous retroperitoneal hematoma), one clinically relevant non-major bleeding (adenovirus induced cystitis and hematuria requiring hospital admission) and one minor bleeding (bruise) event. Catheter-related infection was documented in 4 (36%) patients. No deaths occurred due to CRT or its treatment.
Patients were treated for a minimum of 3 months or longer if the implicated catheter was still in situ. Median treatment time was 3 months (range 2 weeks-7 months). Three patients stopped anticoagulation prior to 3 months (palliation and lost follow-up). None of the CVC was removed as a result of CRT, but 4 were removed for infection, 3 for the completion of chemotherapy, 2 non tunnelled catheters were replaced with long term CVCs, 1 was accidentally dislodged and 1 was removed for logistic reason. The median CVC dwell time was 30 days (range 4-173).
Among the 11 treated patients, 8 patients received platelet transfusions during treatment with LMWH. Eighty seven doses of pooled platelets (or its equivalent) and 64 packed red cells were transfused. Sixteen doses (18%) of platelet transfusions were given to keep platelet count above 20-50 for anticoagulation during the first month of CRT; the remainder were given for clinical indications. Only 4 units (6%) of packed red cells were transfused for major bleeding in one patient while 60 units were used for routine support when hemoglobin was <80 g/L.
Conclusion
Twelve percent of newly diagnosed acute leukemia patients developed CRT. Anticoagulation with LMWH using a dose reduction approach for thrombocytopenia appeared safe and effective with no recurrent VTE events and few bleeding events.
1) Lee AY, Peterson EA. Treatment of cancer-associated thrombosis. Blood. 2013 Oct 3; 122:2310-7
Lee:LEO: Consultancy, Honoraria; Bristol Myers-Squibb: Consultancy, Honoraria, Research Funding; Bayer: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal