Abstract
Introduction: Thrombosis is the second leading cause of death in cancer patients. Hypothetically, prognosis might be improved by preventing thrombotic events by PTP. PTP has to be outweighed with the bleeding risk from PTP benefit. Moreover, PTP in ambulatory cancer patients remains uncertain. We performed a systematic review and meta-analysis of RCTs to determine the risk of major bleeding (MB) and clinically relevant non-major (CRNM) bleeding from PTP with low-molecular weight heparins (LMWH) in solid cancer patients receiving chemotherapy.
Methods: We systematically conducted a comprehensive literature search using MEDLINE and EMBASE databases through May 31, 2016. The RCTs with MB and CRNM bleeding as safety outcomes were included in the analysis. Mantel-Haenszel method was used to calculate the estimated pooled risk ratio (RR), and risk difference (RD) with 95% confidence interval (CI). Random effects model was applied.
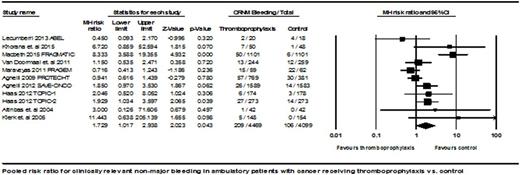
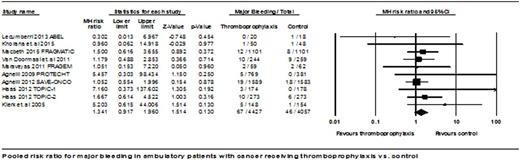
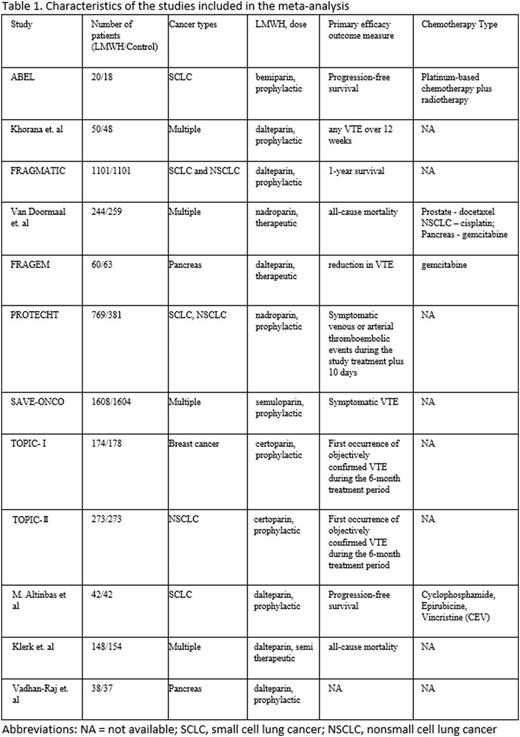
Results: 12 RCTs with a total of 8643 patients were eligible for analysis. Dalteparin, nadroparin, certoparin, semuloparin and bemiparin were used in the studies. 9 studies utilized prophylactic doses, while one used intermediate doses and 2 employed therapeutic dose. The PTP duration was from 6 weeks to 6 months. MB events were reported in 67 (1.486%) patients on PTP compared to 46 (1.112%) in control group. The pooled RR for MB was statistically nonsignificant at 1.341 (95% CI: 0.917 to 1.960, P = 0.130). CRNM bleeding events were noted in 209 (4.637%) in PTP group and 106 (2.563%) in control group. The RR for CRNM bleeding was statistically significant at 1.729 (95% CI: 1.017 to 2.938, P = 0.043). The absolute RD in CRNM bleeding was 0.020 (95% CI: 0.004 to 0.035, P = 0.012) with an estimated number needed to harm (NNH) of 48 to cause one CRNM bleeding event.
Conclusions: Approximately 60 patients are needed to be treated with PTP to prevent one symptomatic venous thrombosis among all ambulatory unselected cancer patients on chemotherapy in a previous meta-analysis. Our meta-analysis revealed that PTP contributed an increase in CRNM bleeding events with NNH of 48. The risk of bleeding should not be underestimated and more RCTs are required before making any recommendations.
Oo:Daiichi Sankyo: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal