Abstract
Introduction: Disseminated intravascular coagulation (DIC) occurs as a complication of many underlying diseases. DIC is characterized by an ongoing systemic activation of the coagulation and fibrinolytic systems, which can exhaust coagulation factors, ultimately leading to bleeding. The International Society of Thrombosis and Hemostasis (ISTH) criteria for DIC consists of a scoring system that includes decreased platelet count, increased D-dimer/Fibrin degradation products, prolonged PT/INR, and decreased fibrinogen. Patients receiving warfarin for anticoagulation also have a prolonged PT/INR. Although the target INR for patients on warfarin is between 2.0 and 3.0, patients may have an INR of less than 2.0 during the initial phase of therapy. The purpose of this study was to compare the coagulopathy observed in patients with DIC and in patients in the initial phase of warfarin therapy.
Methods: Citrated de-identified plasma samples were collected at baseline from patients diagnosed with sepsis-associated DIC (n= 100) and from patients in the initial phase of warfarin therapy (n=100) that were collected under an IRB approved protocol. These plasma samples were evaluated for PT/INR (Recombiplastin, Instrumentation Laboratory, Bedford, MA), APTT (Platelin, Stago, Parsippany, NJ) , fibrinogen (Recombiplastin, Bedford, MA) and functional (Aniara, West Chester, OH) and antigenic levels (Hyphen Biomed, Paris, France) of Factors VII, IX and X.
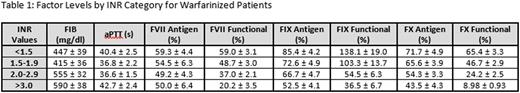
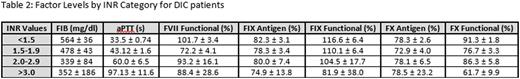
Results: The PT/INR values were statistically significantly higher in warfarinized patients compared to DIC patients (p<0.001). The APTT showed no correlation with the INR in warfarinized patients but increased with an increase in the INR in the DIC group (p<0.001). Similarly, the fibrinogen levels showed no correlation with INR in warfarinized patients; however, in DIC patients, the fibrinogen levels decreased with an increase in the INR. In the factor assays, both the functional and antigenic levels of factors IX and X were decreased in the anticoagulated patients as INR increased, but showed no variation with INR in the DIC patient group. Factor VII levels were decreased with an increased INR in the anticoagulated patients but not the DIC patients. Results for each factor by INR category are shown in Table 1 (warfarinized patients) and Table 2 (DIC patients).
Conclusions: An increase in INR correlated with an increase in APTT and a decrease in fibrinogen in DIC patients but not in patients receiving anticoagulation. Interestingly, in DIC patients, there was no definite tendency in either the functional Factor VII, IX and X or antigen Factor IX or X levels. This contrasts with patients receiving warfarin anticoagulation, where the Factor VII, IX, and X levels all decrease with an increasing INR. In warfarinized patients, changes in coagulation factor levels, but not in global coagulation parameters such as APTT and fibrinogen are demonstrated. However, in DIC greater changes in global coagulation parameters but less consistent changes in factor levels are observed. These results suggest that the coagulopathy observed in a patient with INR ≥ 1.4 is fundamentally different in a patient receiving warfarin for anticoagulation than in a patient with DIC.
Tsuruta:Asahi Kasei Pharma America: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal