Abstract
Thrombotic thrombocytopenic purpura (TTP) is due to a severe deficiency of the von Willebrand factor (vWF) cleaving serine metalloprotease ADAMTS13 and is most commonly diagnosed in adults due to autoantibodies against ADAMTS13. Standard therapy includes plasma exchange (PEX) until platelet counts normalize plus concurrent high dose corticosteroids. In refractory cases, weekly pulse Rituximab for 4 doses is often added. Successful long-term management of relapsing patients beyond these treatments is unclear, in part because the mechanisms for relapsing TTP are unknown. Dysfunctional immunoregulatory systems likely play a role in relapsing disease. Several case series have described disease control following bortezomib therapy (Patriquin 2016). Other immunomodulators including complement pathway and tyrosine kinase inhibitors may prove to offer benefit. Further, supplementing PEX with N-acetylcysteine (Rottenstreich 2016) & Caplacizumab (anti-vWF humanized immunoglobulin) (Peyvandi 2016) has shown promising preliminary clinical results when used to treat an acute episode. Effects on relapse rates with these treatments have not been fully evaluated.
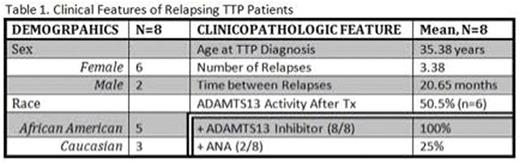
Eight cases of relapsing TTP were identified at MedStar Georgetown University Hospital May 2004 to July 2016. Relapsing TTP was defined as recurrent episode(s) of thrombocytopenia, microangiopathic hemolysis, and confirmed ADAMTS13 activity levels <10% following remission from the initial TTP episode. Retrospective chart review was completed to evaluate demographic and clinicopathologic features, laboratories and treatment at relapse(s), and clinical outcomes.
In our 8 patient cohort, 75% are female (6/8), 62.5% are African American (AA) (5/8), and the mean age at initial TTP diagnosis is 35.38 (range 16-67). The mean number of relapses is 3.38 (range 2-9) with a mean platelet nadir of 45,000/mcL. All patients remain alive. Two are ANA positive, 1 with known systemic lupus erythematosus (SLE) and 1 with suspected SLE. None are HIV positive, and none endorse a family history of TTP. Four identified infections as triggers for their TTP, 1 patient developed TTP during pregnancy and hormonal fertility treatments, and 3 had no identifiable triggers. All had an increased titer of ADAMTS13 inhibitor (Bethesda titer range 0.7 - >8) at the time of relapse(s). Normalization of ADAMTS13 activity was confirmed in most following treatment (n=6), with a mean ADAMTS13 activity level between relapses of 50.5% (range 32-88%). At the time of each relapse, all patients underwent daily PEX with fresh frozen plasma plus high dose corticosteroids for at least 5 days (range 5-21 days), with some requiring gradual PEX weaning over 1-4 weeks and steroid tapering over months based on lab parameters. Two relapsed quickly after PEX discontinuation, both in the setting of systemic illness (lupus flare, cholecystitis). Sequelae of TTP (neurologic, renal, hematologic anomalies) resolved with treatment. All patients received Rituximab therapy during the 1st or 2nd relapse. For the majority (87.5%, 7/8), this intervention did not lead to long-term remission, although 100% (2/2) who transitioned to prophylactic bolus Rituximab every 6 months post splenectomy achieved long-term disease control. It is difficult to distinguish whether remission resulted from maintenance Rituximab, the splenectomy, or a combination of the two. Patients who underwent splenectomy were vaccinated and have not had difficulty with infections or thrombosis.
In conclusion, our cohort of patients with relapsing TTP all had documented ADAMTS13 inhibitors and acutely responded to daily PEX (most requiring PEX wean based on lab parameters) plus high dose corticosteroids. Although Rituximab therapy during initial relapse did not offer a high percentage of long-term remissions, the addition of prophylactic Rituximab every 6 months post splenectomy has achieved long-term control in 2 patients. In our cohort the majority are AA, suggesting genetic susceptibility. HLA/immune transcript levels and ribosomal gene signatures may correlate with TTP disease activity and risk for relapse (Edgar 2015), and could be used to identify high-risk patients in need of more intensive therapy. Given the complexity and severity of this disease, there is an ongoing need for evaluation of relapsing TTP and best strategies for long-term management.
Kessler:Octapharma: Consultancy, Research Funding; Novo Nordisk: Consultancy, Research Funding; Grifols: Consultancy; Genentech: Consultancy, Research Funding; Biogen: Consultancy; Pfizer: Consultancy; Bayer: Consultancy, Research Funding; Baxalta: Consultancy, Research Funding; LFB: Other: Member of DSMB. Broome:True North Therapeutics: Honoraria; Alexion Pharmaceuricals: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal