Abstract
Background: Gaucher disease (GD) is associated with a broad spectrum of signs and symptoms, with phenotypes ranging from fatal perinatal to asymptomatic adult forms. Given the heterogeneous presentation and rarity of the disease, misdiagnosis is common and diagnosis is often delayed, which can lead to avoidable morbidities and potentially irreversible tissue damage. Among the three phenotypes of GD, type 1 is the most prevalent in the Western hemisphere. As part of the global Gaucher earlier diagnosis consensus (GED-C) initiative, we report here the signs and patient co-variables that are regarded by expert physicians as most indicative of type 1 GD in its early stages. The overarching goal of the GED-C initiative is to generate a web-based point-scoring system that can be used by clinicians across specialties to facilitate identification of patients who may benefit from diagnostic testing for GD.
Methods: In an anonymous iterative Delphi process, a panel of expert physicians was asked to provide free-text answers to a series of open questions, including: "Which unexplained signs and co-variables may be important to consider in early type 1 GD?" An independent facilitator categorized responses from round 1 into themes, which were checked and consolidated by the two non-voting co-chairs of the initiative to generate a set of summary factors. In round 2, panel members independently rated the importance of each factor using a 5-point Likert scale (1 = not important, 5 = extremely important). Factors assigned an importance score of at least 3 by more than 75% of respondents were provisionally classified as major; other factors were classified as minor. In round 3, panel members rated their level of agreement with the provisional classification of factors as major using a 5-point pivoted Likert scale (1 = strongly disagree; 3 = neither agree nor disagree; 5 = strongly agree). Consensus was defined as more than 67% of respondents agreeing or strongly agreeing (a score of ≥ 4) with the classification; if consensus was not reached, factors were classified as minor.
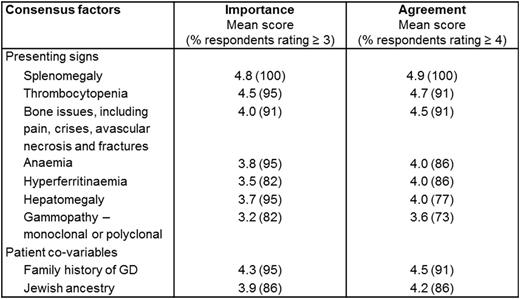
Results: In total, 22 physicians with expertise in type 1 GD were recruited to the GED-C panel from 16 countries. Round 1 (100% response, n = 22) yielded 104 phrases, which were grouped into 38 themes, then consolidated as 21 factors. In round 2 (100% response, n = 22), 10 factors were provisionally classified as major. In round 3 (100% response, n = 22), consensus was reached on 9 major factors in early type 1 GD, including 7 presenting signs and 2 patient co-variables. The mean importance scores (round 2) and agreement scores (round 3) awarded to these 9 major factors are given in Table 1. Minor factors included asthenia, bleeding or bruising, dyslipidaemia, fatigue, gallstones, growth retardation, low bone mineral density and a family history of Parkinson disease.
Table 1. Mean scores of importance and agreement for 9 major factors in rounds 2 and 3, respectively.
Discussion: Definitive diagnostic tests for GD have been available for several years, but patient referral for testing is impeded by several issues, including a general lack of knowledge among clinicians of the signs and co-variables that should arouse a suspicion of GD. The presenting signs and patient co-variables identified by this multidisciplinary consensus initiative will help clinicians to identify those patients who may benefit from diagnostic testing for GD. Several algorithms have been devised with the aim of facilitating GD diagnosis, but these may be perceived as complex by the non-specialist. The next stage of the GED-C initiative will be to use the factors identified here to create a point-scoring system that clinicians of any specialty can use to obtain clear direction regarding the need to test a patient for GD.
Acknowledgment: Submitted on behalf of the GED-C panel members and the European Hematology Association Scientific Working Group 'Quality of Life and Symptoms'. Administration of the GED-C initiative was funded by an unrestricted educational grant from Shire.
Kuter:Amgen: Consultancy; Eisai: Consultancy; Genzyme: Consultancy; GlaxoSmithKline: Consultancy; ONO: Consultancy; Pfizer: Consultancy; Shionogi: Consultancy; Shire: Consultancy; 3SBios: Consultancy; Bristol-Myers Squibb: Research Funding; Protalix: Research Funding; Rigel: Research Funding. Salek:Agios: Consultancy; Servier: Consultancy; Shire: Consultancy; Bristol-Myers Squibb: Research Funding; Novartis: Research Funding; Sanofi: Research Funding. Mehta:Actelion: Honoraria, Other: Travel grants, Research Funding; Genzyme: Honoraria, Other: Travel grants, Research Funding; Protalix/Pfizer: Honoraria, Other: Travel grants, Research Funding; Shire: Honoraria, Other: Travel grants, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal