Abstract
Splenic complications are often seen in pediatric patients with sickle cell disease and could lead to an increase in morbidity and mortality. The most common splenic event is acute splenic sequestration crisis (ASSC) which has been often managed with surgical splenectomy. Although splenectomy has been the treatment of choice for years, the long term complications of splenectomy on vascular events has not been broadly assessed. It has been reported that splenectomy could lead to vascular complications and increased risk of thrombosis in chronic hemolytic conditions. As it was proposed, it could be partially due to the shift form extravascular hemolysis to intravascular leading to the scavenging of nitric oxide (Kato et al, 2007). In terms of cerebral vasculopathy in children with sickle cell disease, screening is usually done by measuring blood flow velocity in the main cerebral arteries using Transcranial Doppler Ultrasonography (TCD). In 2014 Peter Soh and Abdul Siddiqui reported an increased risk of cerebrovascular complications in splenectomized patients with sickle cell disease (3), but it has not been confirmed by other publications. The aim of our study is to evaluate how splenectomy affects cerebral blood flow measured by TCD in patients with homozygous HbS. The secondary aim is to evaluate if Hydroxyurea (HU) has a protective effect on the development of cerebral vasculopathy in splenectomized patients.
We performed a retrospective chart review of patients with sickle cell disease Hb SS and Hb S beta thalassemia followed at the Marian Anderson Center at St. Christopher's Hospital for Children, Philadelphia between 1999 and 2016. In the final analysis we included TCD data on 153 patients, of which 36 had undergone splenectomy. A total of 516 TCD studies were collected, of which 145 patients had a history of splenectomy. Of the 516 TCD assessments in this sample, 70 (13.6%) patients were on HU of which 21 had undergone splenectomy.
Pearson correlations were calculated to explore linear associations of mean cerebral blood flow velocities (CBFV) with age at the time of TCD assessment, time since splenectomy, and TCD values. Associations of CVFV with splenectomy and with HU administration for splenectomy patients were analyzed with analysis of covariance (ANCOVA). The association of time elapsed since splenectomy to TCD measure, adjusting for age at TCD assessment, was explored with multiple linear regression models. Statistical analysis was conducted with SPSS ver. 24.0.
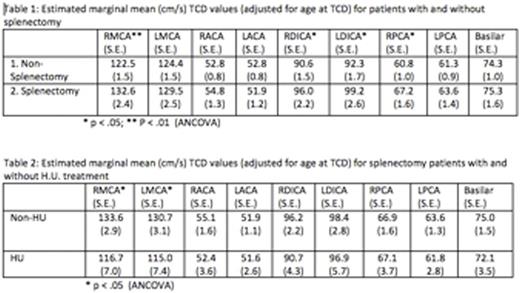
Age at the time of TCD was significantly correlated with mean right cerebral artery (RMCA) (r = -.199, p < .001), LMCA (r = -.181, p < .001), RDICA (r = -.110, p = .047), LDICA (r = -.142, p = .01) and Basilar (r = -.186, p = < .001) velocities. Tables 1 and 2 present estimated mean TCD values (calculated adjusting for age at the time of TCD). In analysis of all TCDs, the estimated mean (RMCA) velocity was significantly higher in patients with history of splenectomy than in patients without splenectomy, (Table 1). There was also significant difference in LDICA, RDICA and right posterior cerebral artery (RPCA) velocities, all of which were higher in splenectomized patients (Table 1). When analyzing the velocities according to time since splenectomy, there were significant associations between years since splenectomy (0-5, 5-10 and >10years) and with both RMCA and LMCA abnormalities. Analysis of TCD results in splenectomized patients on HU versus non-HU, indicates all estimated mean TCDs except for RPCA, are lower for the patients on HU (Table 1), with RMCA and LMCA statistically significant.
Based on our analysis we conclude that in patients with homozygous HbS disease history of surgical splenectomy increases the risk for cerebral vasculopathy. It remains unclear if cerebral vasculopathy develops as a result of splenectomy or if there is a preexisting factor leading to the development of both complications. The other important finding of our study is a protective effect of hydroxyurea on the development of cerebral vasculopathy in splenectomized patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal