Abstract
Introduction:The prognosis of patients with hematologic malignancies (HM) admitted to intensive care units (ICU) is historically poor due to complications of treatment and disease progression with reported overall mortality rates of 24.3% to 84.1%. There is little known regarding predictive variables for ICU admission in adult patients with HM.
Objective: Our primary objective was to audit the clinical outcomes including mortality of our HM patients admitted to any hospital ICU unit and compare their characteristics and outcomes with non-ICU hospitalized patients. A secondary objective was to identify the predictive factors for ICU admission and survival.
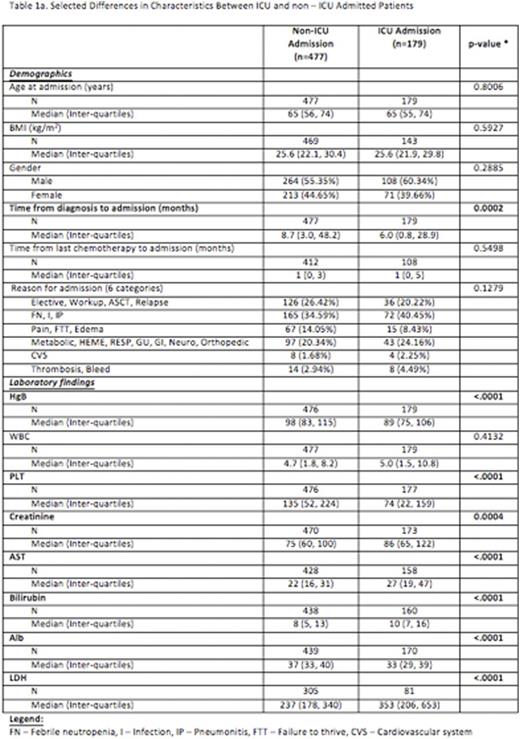
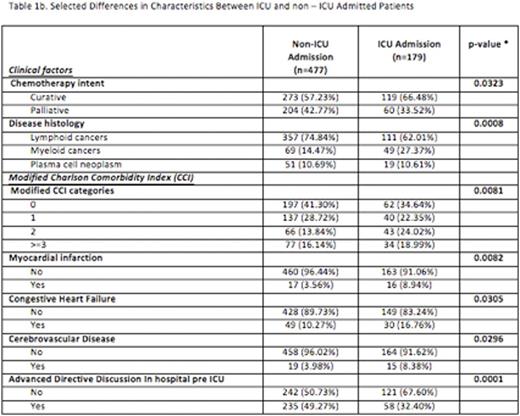
Methods: In this single centre retrospective study, we audited 656/2141 consecutive patients with HM who were admitted to our hospital from 2009-2015 and compared the disease, patient characteristics, and clinical outcomes of HM patients who did or did not get admitted to any ICU. We excluded patients admitted for palliative care and in instances where the patient was admitted more than once, we included only the most recent admission. We enriched for patients who were admitted to the ICU over this 6-year period to improve the statistical power of comparing these two populations. The variables considered included: reason for admission, underlying diagnosis, the modified Charlson Comorbidity Index (CCI), selected laboratory parameters at admission to hospital, previous chemotherapy type, line of treatment, timing and intent, body mass index (BMI), GSCF use, age and sex. We also screened for electronic documentation of advanced directives preceding ICU or hospital admission. We compared the characteristics of ICU (n=179, 27%) and non ICU (n=477, 73%) admitted patients using the Fisher exact test and Wilcoxon rank-sum non parametric test for categorical and continuous variables, respectively. To search for the significant predictive factors for ICU admissions and mortality, univariate and multivariate logistic regression analyses were used.
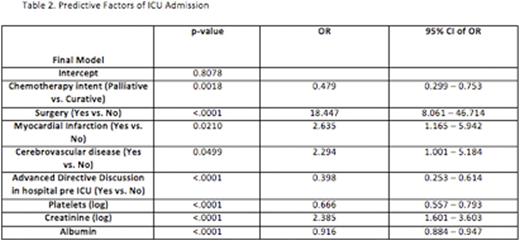
Results: Over the 6-year period, the admission rate to any ICU for HM patients was 9.4%. Median age of the 656 patients was 65.0 (IQR 55-74) and 57% were male with a median time from last chemotherapy and diagnosis of 1 month (IQR 0-3) and 7.8 months (IQR 2.3-44), respectively. Selected patient and disease characteristics comparing ICU and non- ICU admitted patients are in Table 1. There were no differences in median age, BMI, gender, time from last chemotherapy, reasons for admission, WBC, and line of chemotherapy. Patients admitted to any ICU were more likely to have received chemotherapy with curative intent (p=0.0323) and have myeloid cancers (p= 0.0008). They had shorter times from diagnosis, lower hemoglobin, platelet and albumin levels but higher creatinine levels, lactate dehydrogenase (LDH) and liver enzymes. ICU admitted patients had higher CCI scores and in particular history of cardio/cerebro-vascular disease. They also had lower rates of advanced directives (32% vs 49%, p=0.0001). 50% of ICU patients were mechanically ventilated and 25% received vasopressors. Median length of hospital stay was 19 days for ICU and 6 days for non-ICU patients and median ICU length of stay was 3 days (IQR 2-6 days). 34 patients (19.0%) died in ICU and but in hospital mortality was 33% (compared with 8% for non ICU). In the multivariate analysis, six covariates significantly related to ICU admission: chemotherapy intent (curative vs. palliative), history of myocardial infarction, lower platelets, creatinine and albumin levels and no advanced directives (Table 2). Median overall survival was 4.7 months vs. not yet reached for ICU and non ICU admitted patients respectively. 30-day and 6-month survivals were 67% and 47% (ICU) compared with 89%, and 77% in non-ICU admitted patients. The predictors of death in ICU admitted patients were male sex (OR 2.6, 95% CI 1-6.7, p =0.03) and mechanical ventilation (OR 6.55, 95% CI 2.6-18.5, p=0.0001).
Conclusions:We validate the previously reported high rates of ICU mortality for patients with hematologic malignancies and have identified the risk factors for ICU admission. Patients without advanced directives have a high likelihood for admission to ICU and potentially represent a targetable group for interventions to avoid inappropriately aggressive care. A predictive score is in development to help identify the patients warranting closer scrutiny and goals of care discussions.
Buckstein:Celgene: Honoraria, Research Funding; Novartis: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal