Abstract
Background
Neutropenic enterocolitis (NEC) is an abdominal infection reported in patients with acute myeloid leukemia (AML) following chemotherapy, especially cytarabine. Specific data regarding the impact of different cytarabine schedules and antibacterial regimens for NEC are sparse.
Aims
The aim of this study was to provide an update on therapeutic interventions of NEC. Predictors of mortality and determinants of favorable outcome at 30 days after NEC onset were considered, and finally we focused on the optimal antibiotic strategy for the preemptive therapy of NEC
Methods
NEC episodes were retrospectively pinpointed among 440 patients with newly diagnosed AML hospitalized in our institution, from 1 January 2002 to 31 December 2012, for receiving chemotherapy protocols with cytarabine. Two subgroups, survivors versus non-survivors, were compared to identify the predictors of outcome within 30-days of NEC onset. Finally, an optimal antibiotic strategy for front-line NEC treatment was suggested.
Patients with severe neutropenia and clinical signs suggestive of NEC, i.e. fever (axillary temperature ³38¡C), diarrhea (>1 stool daily) and/or abdominal pain, were under strict ultrasonographic monitoring. Patients positive at US examination for pathologic bowel wall thickening (>4 mm in transversal scans for at least 30 mm length) were diagnosed with NEC, according to standardized criteria.
The following variables were selected for the statistical analysis: antileukemic protocols [containing standard-dose (100 mg/m2 daily for at least 7 days), intermediate-dose (200 mg/m2 daily for at least 7 days), and high-dose (2000 to 6000 mg/m2 daily for at least 4 days) cytarabine], ultrasonographic features, microbiological findings, antibacterial therapy (front-line antibiotic treatments of febrile neutropenia that spared tigecycline, and the number and type of antibiotics definitively used after NEC diagnosis), adjunct therapeutic modalities (systemic antifungal therapy, G-CSF, bowel rest and total parenteral nutrition), and severe neutropenia resolution.
Results
NEC was documented in 100 (23.8%) of analyzed patients: 42.5% had received high-dose cytarabine while 19% and 15% intermediate-dose and standard-dose cytarabine, respectively (P<0.001). The 30-day NEC attributable mortality was 23%.
In univariate analysis, patients in the non-survivor subgroup were more likely to have received induction chemotherapy courses based on high-dose cytarabine (P< 0.001) and NEC treatment with tigecycline-sparing ²2-antibiotic regimens. In fact, the 23 patients who died included 13 of the 37 patients (35.1%) whose antibacterial regimens consisted of 2-antibiotic combinations and 10 of the 63 patients (15.8%) who were on 3-antibiotic combination regimens (P= 0.027). The only multidrug regimen that was significantly more common in the survivor subgroup (P= 0.036) was the combination of tigecycline, meropenem and daptomycin.
In multivariate analysis, high-dose cytarabine-containing chemotherapy was the independent predictor of poor outcome (OR: 0.089; 95%CI: 0.024-0.329; P<0.001), whereas NEC therapy with a combination of three specific antibiotics (tigecycline, meropenem and daptomycin) was associated with a favorable outcome (OR: 5.096; 95%CI: 1.516-17.131; P=0.008).
Conclusion
Chemotherapy schedules with vigorous dosages of cytarabine for AML remission are associated with a high rate of NEC incidence and attributable mortality. Prompt initiation of combined therapy with regimens of different antibiotic classes which have synergistic activity against complicated intra-abdominal infections, specifically those including tigecycline, may be particularly effective in improving 30-day survival rate after NEC onset.
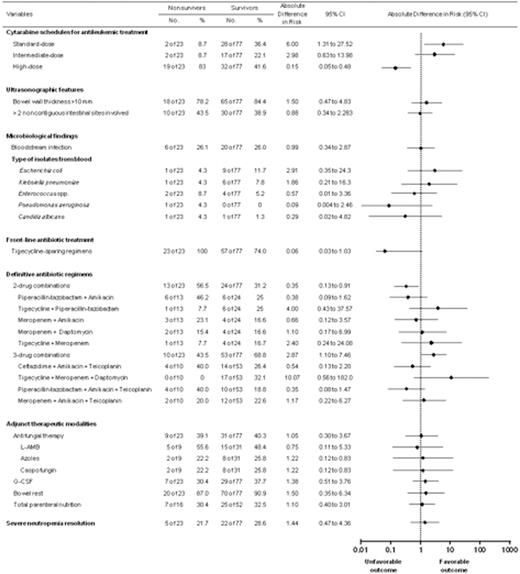
Subgroup analyses of overall survival for several variables associated with death among the entire patient population with neutropenic enterocolitis. Rates and absolute differences in the risk of mortality are given.
Subgroup analyses of overall survival for several variables associated with death among the entire patient population with neutropenic enterocolitis. Rates and absolute differences in the risk of mortality are given.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal