Abstract
Background: Disparities in MM survival among different racial groups persist despite improvements in overall survival (OS). We report a comprehensive review of the SEER Medicare database to elucidate the causes of differences in disease presentation, management practices, cost of care and their relationships to outcomes among the MM patients (pts) from different racial groups.
Methods: Pts diagnosed with MM between 1991-2010 with continuous Medicare coverage (1 year prior to diagnosis-date of death/end of 2012) were included. MM complications (MM-C); hypercalcemia (C), renal dysfunction (R), anemia (An), bone fractures (B), dialysis (D) occurring prior to/within 30 days of MM diagnosis (at diagnosis; AT-D), or any time later (after diagnosis; AF-D) were summarized. Demographics, survival (PEDSAF files) and disease characteristics, drug/stem cell transplant (SCT) utilization (NCH, OUTSAF, PDESAF files) were obtained. Trends in incidence of MM-C, treatment type over time (proportional odds) and their association with race (logistic regressions) were compared. Associations between race, MM-C AT-D and MM related death using Fine and Gray's competing risk methods were analyzed. Medicare claims adjusted for inflation (2013) within the first 6 months (mth)/total MM care were summed by drug and total charges. Median cost of care by race and year of diagnosis were evaluated by Kruskal-Wallis (univariate) and proportional odds models (multivariate).
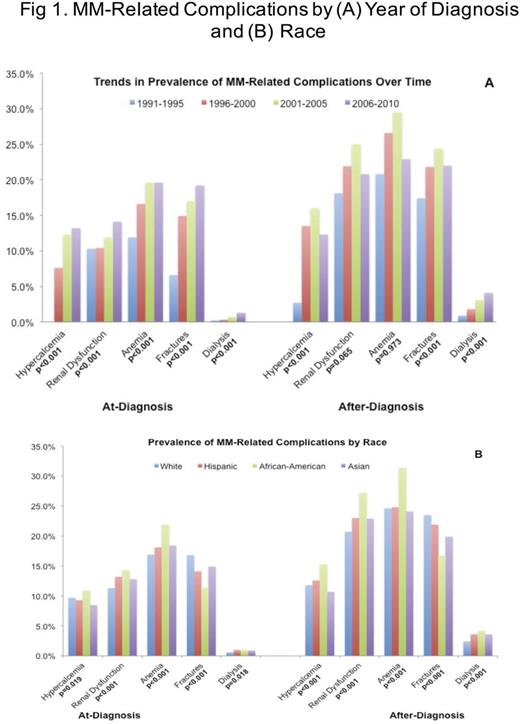
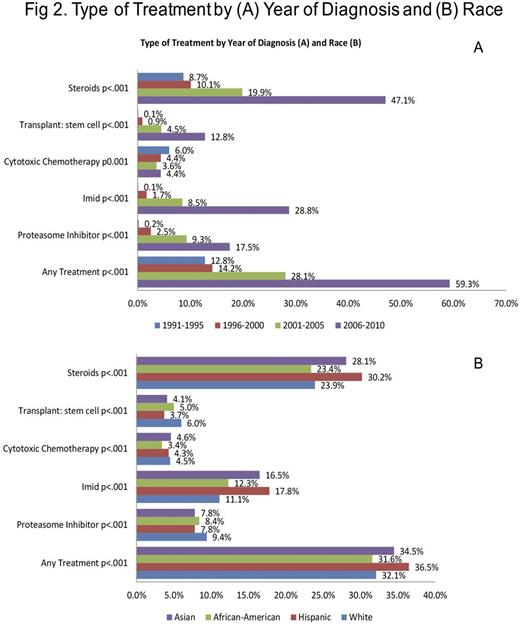
Results: A total of 35842 pts (52.1% males) with median age of 76 yr (range 18-104) were included. Mutually exclusive racial subgroups were: White (W, 72%), Hispanic (H: 7.3%), African-American (AA, 16.2%), Asian (A, 4.1%), other (0.3%). A significantly increasing trend in the prevalence of all MM-C AT-D was seen over time (all p<0.001). For AF-D, all MM-C initially increased but decreased from 2006-2010 except D that showed continued increase (Fig 1A). For race, MM-C were significantly different, with AA having the most C, R, An and D while W having the most B (Fig 1B). Inferior OS was seen with male gender (p=0.006), increasing age, earlier years of diagnosis, belonging to W or H race, C, R and B (all p<0.001), but not with An (p=0.298) or D (p=0.378). Trends in OS over time showed a significant interaction with race in 1991-1995 (p<0.001), 1996-2000 (p=0.004) and 2001-2005 (p<0.001) but not in 2006-2010 (p=0.182), possibly due to shorter follow up. Medicare claims analysis showed that pts receiving any treatment increased from 12.8% in 1991-1995 to 59.3% in 2006-2010 (p<0.001). Specific therapy utilization, including SCT and all drug classes/agents evaluated increased except for cytotoxic chemotherapy utilization (melphalan/cyclophosphamide), which decreased (Fig 2A). Any therapy utilization was significantly different by race (p<0.001) with highest for H (36.5%) and lowest for AA (31.6%). Specific treatments differed significantly by race (Fig 2B). Cost of care analysis showed significant increase over years for median drug claims (0.23k to 3.63k) and total claims (5.11k to 27.8k) during first 6 mth as well as for any time after MM diagnosis (drug: 1.3k to 9.9k, total: 21.9k to 84k) (p<0.001 for all). Median drug claims in first 6 mth were highest among AA (1.3k) and lowest among A (0.63k) (p<0.001). Same was true for total claims in first 6 mth (p<0.001). For any time after diagnosis, H had the highest drug (p<0.001) and total (p=0.081) claims. There were significant interactions between year of diagnosis, race and cost of care with H seeing the highest increase in drug claims in first 6 mth (p<0.001) and any time (p=0.002).
Conclusion: MM-C have generally decreased AF-D due to improved therapeutics although AA continue to have the highest rates of MM-C. Our data shows that utilization and cost of MM care have increased tremendously with resulting improved outcomes, but significant racial disparities persist. These disparities may be in part due to impaired access to new agents from lack of supplemental insurance for certain racial groups. Drug utilization and cost of care disparities may also be due to differences in co-morbidities, MM-C or access leading to differential healthcare utilization and should be explored in order to ameliorate disparities in outcomes.
Ailawadhi:Pharmacyclics: Consultancy; Novartis: Consultancy; Amgen Inc: Consultancy; Takeda Oncology: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal