Abstract
Introduction
Pre-transplant risk assessment is a crucial issue to improve the HCT decision-making process. Several transplant-related models have been designed to optimize decision-making about suitable candidates for allogeneic HCT. The refined Disease Risk Index (DRI) was developed to stratify disease risk acrosshistologiesand HCT regimens. However, few recipients of haploidentical HCT were originally included in the DRI study cohorts. In 2015 a first large cohort of non-myeloablativehaploidentical HCT with post-transplant cyclophosphamide (PTCy) confirmed the validity of DRI also in this setting.
Beside this, in the past few years the novel composite end point of GVHD-free, relapse-free survival (GRFS) after HCT spreads out. GRFS acknowledge that both survival and rates of grade 3-4 acute GVHD, chronic GVHD requiring systemic treatment, relapse, or death are clinically meaningful. GRFS therefore represents ideal recovery from HCT and a measure of cure without ongoing morbidity.
Methods
We analyzed risk-stratified GRFS according to the refined DRI in haploidentical HCT at our Center, where it was exploited - since 2006 - asirolimus-based,calcineurininhibitor-free prophylaxis of GvHD to allow the safe infusion of unmanipulated haploidentical HCT.
We analyze data collected between 2006 and 2014 including 207 adult pts. Data were prospectively collected in Institutional database. A written consent was given by pts allowing the use of medical records for research in accordance with the Declaration of Helsinki.
All consecutive pts receiving a haplo HCT as 1st allogeneic transplantation were included - pts receiving haplo HCT as 2nd or 3rd HCT were excluded from the present analysis.
Results
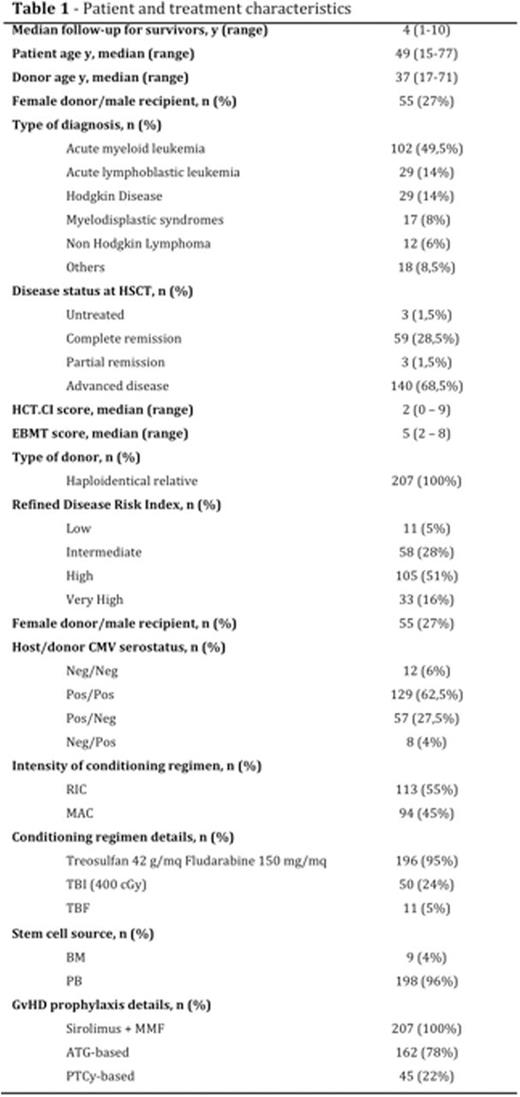
Baseline characteristics of the 207 pts are outlined in table 1.
With 4-year median follow-up, 4-year probabilities of transplant related mortality (TRM),relapse, progression-free survival (PFS), and overall survival (OS) were 25,8%, 42,5%, 31,7%, and 34,4%, respectively. Day-100 cumulative incidence of grade II-IV and III-IV acute graft-versus-host-disease (GvHD) were 30,1% and 15,5% respectively. The 4-year cumulative incidence of chronic GvHD was 33,5% (moderate-severe chronic GvHD 26,2%).
Considering the composite end point of GRFS, for the entire population the 4-year GRFS was 17,8%.
By refined DRI group, low-intermediate (n 69), high (n 105), and very high (n 33) risk groups had 4-year GRFS estimates of 31,1%, 13,7%, and 3,0% (p < .0001), with corresponding 4-year OS estimates of 56,7%, 28,9%, and 6,1% (p < .0001).
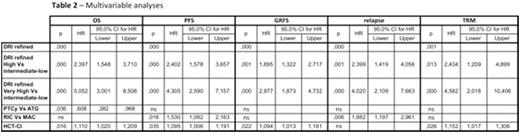
On a multivariable Cox model we considered as covariates age, host/donor sex mismatch, host/donor CMV status, stem cell source, conditioning intensity, GvHD prophylaxis ATG-based versusPTCy-based, DRI stratification, HCT Comorbidity Index Score (HCT-CI).
On multivariable analyses, the DRI was statistically significantly associated with GRFS, OS, PFS, relapse, TRM and grade II to IV acute GvHD (ref table 2).
HCT-CI was statistically significantly associated with GRFS, OS, PFS and TRM. Conditioning intensity was associated with PFS and relapse, while GvHD prophylaxis (PTCyvs ATG) was only associated with OS.
Interestingly no risk factors were clearly emerging for chronic GvHD.
Conclusions
The combination of a refined DRI and GRFS provide a valid tool to improve the HCT decision-making process and will help optimize patient outcomes.
Ciceri:MolMed SpA: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal